Sexually transmitted epididymo-orchitis is an inflammatory condition involving the epididymis and testicle, typically caused by sexually transmitted infections (STIs) such as Chlamydia trachomatis and Neisseria gonorrhoeae. It primarily affects sexually active men under 35 years of age and represents a urologic emergency requiring prompt recognition and management to prevent complications such as infertility or abscess formation.
Etiology and Pathophysiology of Epididymo-Orchitis from STIs
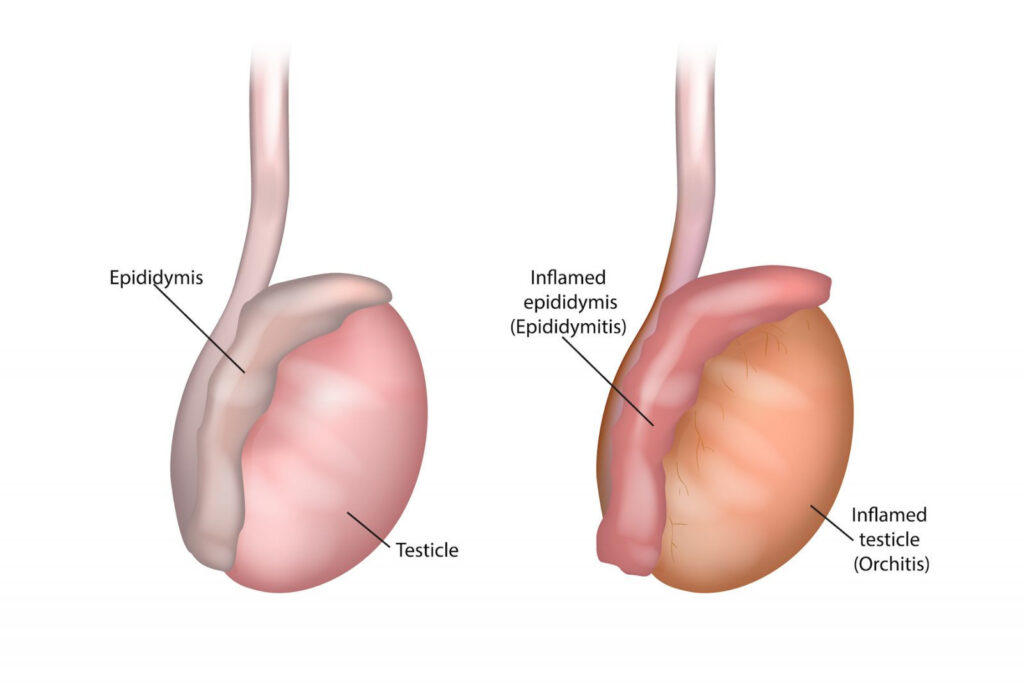
Sexually transmitted pathogens ascend from the urethra or bladder through the vas deferens to infect the epididymis, with secondary inflammation of the testicle (orchitis). The infection leads to localized edema, hyperemia, and infiltration of neutrophils, causing pain and swelling in the scrotum.
Common Causative Agents
- Chlamydia trachomatis: Most frequent cause in men <35 years.
- Neisseria gonorrhoeae: Frequently co-infects with chlamydia.
- Mycoplasma genitalium: Emerging cause with antibiotic resistance.
- Enteric bacteria (e.g., E. coli): Rarely sexually transmitted; more common in older men or those with urinary abnormalities.
Risk Factors for STI-Related Epididymo-Orchitis
- Age under 35 years
- New or multiple sexual partners
- Unprotected intercourse
- History of prior STIs
- Inconsistent condom use
- Urethritis or prostatitis
- Men who have sex with men (MSM)
Clinical Presentation and Symptoms
Patients typically present with:
- Acute unilateral scrotal pain and swelling
- Scrotal erythema and tenderness
- Dysuria or urethral discharge
- Fever and systemic symptoms (in severe cases)
- Pain radiating to the groin or lower abdomen
On physical examination:
- Tender and swollen epididymis and/or testicle
- Positive Prehn’s sign (relief of pain upon scrotal elevation)
- Possibly a palpable epididymal tail or thickened spermatic cord
Diagnostic Evaluation
Laboratory Investigations
- Urinalysis and urine culture: Pyuria or bacteriuria may be present.
- Nucleic Acid Amplification Tests (NAATs): Gold standard for detecting Chlamydia and Gonorrhea in urine or urethral swabs.
- Urethral swab: Indicated if discharge is present.
- HIV and syphilis serology: Routine in STI evaluations.
Imaging
- Scrotal ultrasound with Doppler: Essential for diagnosis; reveals increased blood flow (hyperemia), enlarged epididymis/testicle, and may rule out testicular torsion.
Differential Diagnosis
- Testicular torsion: Surgical emergency; must be ruled out urgently.
- Inguinal hernia
- Testicular tumor
- Hydrocele or varicocele
- Idiopathic scrotal edema
Evidence-Based Treatment of Sexually Transmitted Epididymo-Orchitis
Antibiotic Therapy
Empiric treatment should target both Chlamydia and Gonorrhea:
CDC-Recommended Regimen (2024 Update):
- Ceftriaxone 500 mg IM single dose (1 g if >150 kg body weight)
plus - Doxycycline 100 mg orally twice daily for 10 days
Note: Azithromycin is no longer preferred due to resistance trends.
If Mycoplasma genitalium is suspected:
- Consider Moxifloxacin 400 mg orally daily for 7–14 days
Adjunctive Management
- Scrotal support and bed rest
- NSAIDs for pain and inflammation (e.g., ibuprofen)
- Avoidance of sexual activity until treatment completion and symptom resolution
- Partner notification and testing
Prevention and Patient Education
Safe Sex Practices
- Consistent condom use
- Mutual monogamy or limiting sexual partners
- Routine STI screening for sexually active individuals
Partner Management
- Sexual partners from the past 60 days should be notified, tested, and treated.
- Abstinence until partners are fully treated is essential to prevent reinfection.
Follow-Up
- Reassessment in 3–7 days to ensure clinical improvement
- Repeat NAAT testing after 3 months due to high reinfection risk
Complications of Untreated Epididymo-Orchitis
- Infertility due to testicular atrophy or scarring
- Abscess formation requiring drainage
- Chronic epididymitis
- Systemic infection or sepsis (in severe cases)
- Reactive hydrocele
Special Considerations
MSM and HIV-Positive Patients
- Increased risk of coinfection with multiple STIs, including syphilis and hepatitis B.
- Broader STI panel testing is warranted.
- Treatment regimens remain the same unless complications arise.
Pediatric and Older Populations
- Rarely due to STIs; more commonly associated with urinary tract anomalies or prostatitis.
FAQs
What is the most common cause of sexually transmitted epididymo-orchitis?
Chlamydia trachomatis is the leading cause in sexually active men under 35.
How is it different from bacterial (non-STD) epididymitis?
Non-STD cases often involve enteric organisms and occur in older men with urinary tract issues.
Can sexually transmitted epididymo-orchitis be cured?
Yes, with appropriate antibiotics and early intervention, most cases resolve completely.
Should sexual partners be treated?
Yes, to prevent reinfection and stop the spread of STIs.
Can this lead to infertility?
If left untreated or recurrent, inflammation and scarring can impair sperm function and fertility.

