Severe thrombocytopenia in refractory chronic immune thrombocytopenic purpura (ITP) represents a challenging clinical entity marked by persistent low platelet counts, often <30×10⁹/L, despite multiple lines of therapy. Refractory ITP is diagnosed when patients fail to respond to splenectomy or exhibit ongoing bleeding risk due to severely depressed platelet levels. This condition necessitates personalized, multi-modal treatment strategies.
Pathophysiology of Refractory Chronic ITP
Immune-Mediated Platelet Destruction and Impaired Production
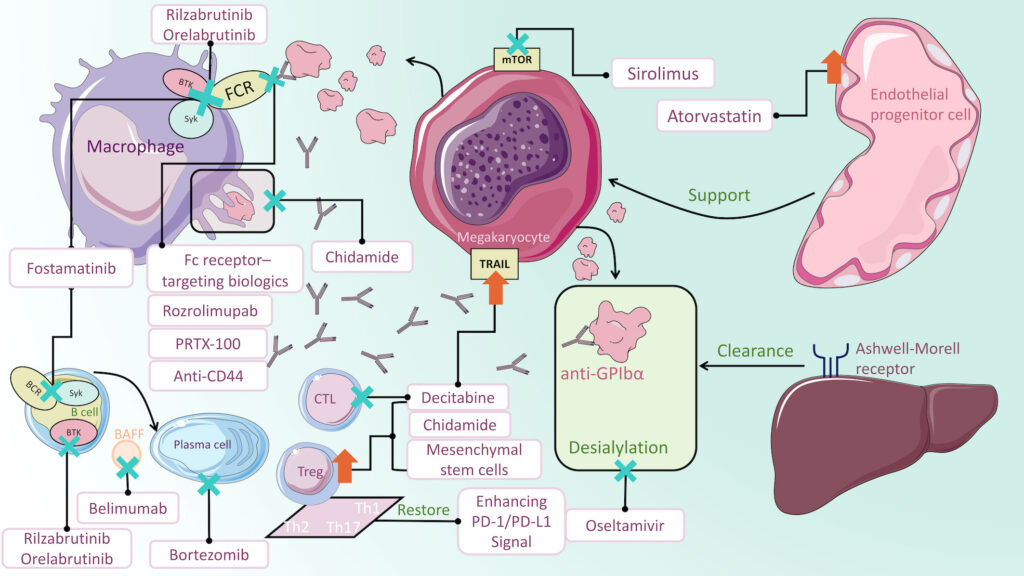
The hallmark of chronic ITP is an autoimmune response against platelet surface glycoproteins (e.g., GPIIb/IIIa), resulting in enhanced clearance by splenic macrophages. In refractory cases, impaired megakaryopoiesis further exacerbates thrombocytopenia. T-cell dysfunction, autoantibody persistence, and chronic inflammation perpetuate platelet destruction despite standard interventions.
Diagnostic Criteria and Evaluation of Refractory ITP
Diagnostic Features
- Platelet count persistently <30×10⁹/L.
- Duration >12 months despite therapy.
- Non-responsiveness to corticosteroids, IVIG, and splenectomy.
- Exclusion of secondary causes (e.g., SLE, HIV, HCV, lymphoproliferative disorders).
Workup for Refractory Status
- Bone marrow biopsy to assess megakaryocytes.
- Direct antiglobulin test to rule out Evans syndrome.
- Flow cytometry for T-cell dysregulation and lymphocyte profiling.
- Serum thrombopoietin levels.
First-Line and Failed Therapies in Chronic ITP
Common Initial Treatments
- Corticosteroids (e.g., prednisone, dexamethasone): Often effective initially but not durable.
- Intravenous Immunoglobulin (IVIG) and Anti-D: Temporarily raise platelet count.
- Splenectomy: Curative in some but ineffective in truly refractory patients.
Failure of these treatments defines the refractory phase and warrants advanced interventions.
Second-Line Therapies for Refractory Chronic ITP
Rituximab: B-Cell Depletion Strategy
Rituximab, an anti-CD20 monoclonal antibody, suppresses autoantibody production and modifies the immune environment. Though initial response rates reach 60–70%, long-term remissions occur in a minority.
Thrombopoietin Receptor Agonists (TPO-RAs)
TPO-RAs stimulate megakaryocyte proliferation and platelet production, effectively countering both immune destruction and impaired platelet synthesis.
- Eltrombopag: Oral, hepatically metabolized; dose-adjusted in hepatic impairment.
- Romiplostim: Subcutaneous injection; suited for patients intolerant to oral agents.
- Avatrombopag: Favorable pharmacokinetics and fewer dietary restrictions.
These agents frequently achieve sustained platelet response in refractory patients.
Third-Line and Rescue Strategies
Immunosuppressive Agents
- Mycophenolate mofetil, azathioprine, and cyclosporine offer modest benefit in refractory cases with autoimmune overlap.
- Dapsone and vincristine are occasionally used as steroid-sparing agents.
Splenectomy in the Refractory Setting
Though typically second-line, delayed splenectomy may still benefit selected patients with splenic sequestration predominance and no contraindications.
Experimental Therapies
- FcRn inhibitors (e.g., efgartigimod) block IgG recycling, reducing autoantibody levels.
- BTK inhibitors target B-cell signaling and have shown early promise in clinical trials.
- Low-dose decitabine is under investigation for T-cell modulation.
Bleeding Risk and Supportive Management in Severe Thrombocytopenia
Hemostasis Monitoring
- Active bleeding or platelet counts <10×10⁹/L necessitate urgent intervention.
- Platelet transfusions are reserved for life-threatening hemorrhage due to rapid destruction.
Adjunctive Measures
- Antifibrinolytics (e.g., tranexamic acid) during mucosal bleeding.
- Hormonal suppression in menstruating females to mitigate menorrhagia.
- Avoidance of NSAIDs and antiplatelet agents.
Prognosis and Long-Term Monitoring
Predictive Factors for Poor Response
- Older age, presence of autoimmune comorbidities, and prolonged disease course.
- Lack of early response to rituximab or TPO-RAs.
Monitoring Parameters
- Regular CBCs and hepatic function panels during TPO-RA use.
- Bone marrow reassessment if cytopenias evolve or transformation is suspected.
Multidisciplinary Care Approach
Management of severe thrombocytopenia in refractory chronic ITP requires integration of hematologists, immunologists, and supportive care teams. Patient education, risk mitigation, and tailored treatment regimens enhance therapeutic success and quality of life.
FAQs
What defines refractory ITP?
Refractory ITP is defined by failure to respond to splenectomy and other standard therapies, with persistently low platelet counts and/or bleeding.
Can refractory ITP be cured?
While a definitive cure is rare, long-term remission is possible with advanced immunotherapies or TPO-RAs.
How effective are TPO receptor agonists in refractory ITP?
TPO-RAs can induce a durable platelet response in up to 80% of patients with refractory disease.
Is splenectomy always ineffective in refractory ITP?
Not always. Selected patients without autoimmune overlap may still benefit from splenectomy as a delayed intervention.
What is the role of rituximab in chronic refractory ITP?
Rituximab is often effective short-term, especially in early refractory stages, but long-term remission rates are lower than with TPO-RAs.

