Severe recalcitrant psoriasis is a chronic, immune-mediated inflammatory disorder characterized by thick, scaly plaques that persist despite conventional therapy. This condition represents a subset of psoriasis cases resistant to topical agents, phototherapy, and even systemic medications. Persistent inflammation, patient-specific immune responses, and comorbidities complicate treatment outcomes. A structured, individualized therapeutic approach is imperative for effective long-term control.
Clinical Manifestations and Diagnostic Considerations
Key Features of Recalcitrant Psoriasis
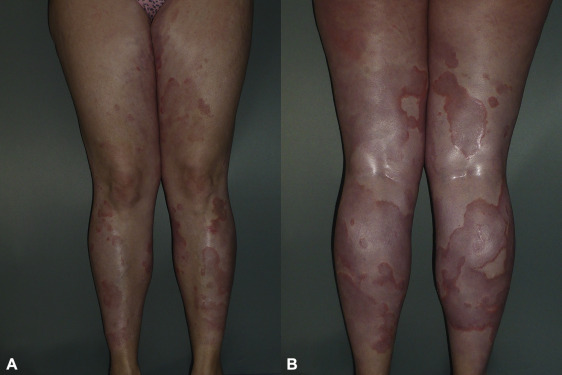
- Widespread Plaques: Symmetrical, thick, erythematous plaques with silvery scale.
- Treatment Resistance: Poor or no response to corticosteroids, methotrexate, or UVB therapy.
- Frequent Flares: Triggered by stress, infections, medications, or abrupt cessation of therapy.
- Associated Symptoms: Intense pruritus, pain, cracking, and bleeding of affected skin.
Diagnostic Criteria
- Chronicity of more than 6 months.
- PASI (Psoriasis Area and Severity Index) score ≥ 10 despite systemic therapy.
- Negative response to two or more standard treatments.
Etiopathogenesis of Recalcitrant Psoriasis
Immune Dysregulation
- Overactivation of T-helper 17 (Th17) and Th1 pathways leads to excessive production of interleukins (IL-17, IL-23, TNF-α).
Genetic Susceptibility
- HLA-C*06:02 allele association with early-onset, severe psoriasis.
Environmental and Lifestyle Triggers
- Obesity, smoking, alcohol intake, psychological stress, and mechanical trauma (Koebner phenomenon).
Drug-Induced Exacerbation
- Beta-blockers, lithium, antimalarials, and rapid corticosteroid withdrawal may precipitate severe flares.
Escalation Strategies for Resistant Psoriasis
Optimizing Topical Therapy
- Combination Products: Calcipotriene + Betamethasone dipropionate.
- Occlusion Therapy: Enhances corticosteroid penetration in hyperkeratotic lesions.
- Keratolytics: Salicylic acid to reduce scale and enhance drug absorption.
Phototherapy Adjustments
- Narrowband UVB (NB-UVB): Preferred for extensive, stable disease.
- PUVA (Psoralen + UVA): Considered for recalcitrant plaques unresponsive to NB-UVB.
- Excimer Laser: Targeted treatment for localized thick plaques.
Systemic Therapies for Severe Recalcitrant Psoriasis
Conventional Systemic Agents
- Methotrexate: Anti-inflammatory and immunosuppressive; dose adjustments may be needed for inadequate response.
- Cyclosporine: Rapid action, ideal for flare control; limited by nephrotoxicity with prolonged use.
- Acitretin: Used in combination with phototherapy for synergistic effects.
Biologic Therapies: Next-Level Precision
Biologics target specific immune pathways, offering improved outcomes in resistant psoriasis.
| Biologic Class | Target | Example Drugs |
|---|---|---|
| TNF-α inhibitors | TNF-α | Etanercept, Infliximab |
| IL-12/23 inhibitors | IL-12 & IL-23 | Ustekinumab |
| IL-17 inhibitors | IL-17A | Secukinumab, Ixekizumab |
| IL-23 inhibitors | IL-23 | Guselkumab, Tildrakizumab |
Treatment Monitoring
- Baseline and routine labs: CBC, LFTs, lipid profile, TB screening.
- Assess PASI and DLQI (Dermatology Life Quality Index) every 12–16 weeks.
Novel and Emerging Therapies
Janus Kinase (JAK) Inhibitors
- Oral agents like Tofacitinib and Upadacitinib show promise but carry infection and malignancy risk.
TYK2 Inhibitors
- Deucravacitinib, a selective TYK2 inhibitor, offers targeted modulation of IL-23 and IL-12 signaling.
Apremilast (PDE4 Inhibitor)
- Useful in patients unable to tolerate systemic immunosuppression; moderate efficacy but good safety profile.
Managing Flares and Long-Term Maintenance
Relapse Prevention
- Gradual tapering of systemic therapy.
- Patient education on trigger avoidance and adherence.
Comorbidity Screening
- Psoriatic arthritis, metabolic syndrome, cardiovascular disease, depression.
Nutritional and Lifestyle Support
- Anti-inflammatory diet, weight loss, smoking cessation, and regular physical activity support remission.
Psychosocial Impact and Support Strategies
Severe psoriasis significantly affects self-esteem, social interactions, and mental health. Integrated care involving dermatologists, psychologists, and support groups fosters holistic management. Cognitive behavioral therapy and stress reduction techniques aid in controlling flare frequency.
FAQs
What qualifies psoriasis as “recalcitrant”?
Psoriasis is considered recalcitrant when it fails to improve after multiple systemic therapies, including biologics or phototherapy.
Can biologics cure severe psoriasis?
Biologics control inflammation effectively, but psoriasis is chronic. Continuous therapy or monitoring is needed to maintain remission.
How long does it take for biologics to show results?
Most biologics show significant skin clearance within 12–16 weeks, depending on the drug and patient response.
Is severe psoriasis linked to other health conditions?
Yes. It is associated with comorbidities like psoriatic arthritis, diabetes, obesity, and cardiovascular disease.
Are there any natural or supportive remedies for resistant psoriasis?
While not a replacement for medical treatment, omega-3 fatty acids, vitamin D, and mindful lifestyle changes may complement conventional care.

