Severe pre-eclampsia is a life-threatening hypertensive disorder of pregnancy, typically emerging after 20 weeks of gestation. Characterized by sustained high blood pressure (≥160/110 mmHg) and evidence of end-organ dysfunction, it presents a critical threat to maternal and fetal health. Unlike mild forms, severe pre-eclampsia demands immediate and aggressive intervention to prevent progression to eclampsia, HELLP syndrome, or fetal compromise.
Diagnostic Criteria for Severe Pre-Eclampsia
According to ACOG (American College of Obstetricians and Gynecologists) and WHO guidelines, severe pre-eclampsia is diagnosed in the presence of one or more of the following:
- Systolic BP ≥160 mmHg or Diastolic BP ≥110 mmHg on two occasions, 4 hours apart
- Proteinuria ≥5 g in 24-hour urine or Protein/Creatinine ratio ≥0.3
- Thrombocytopenia: Platelet count <100,000/mm³
- Elevated liver enzymes with right upper quadrant or epigastric pain
- Renal insufficiency: Serum creatinine >1.1 mg/dL
- Pulmonary edema
- New-onset cerebral or visual disturbances
Pathophysiology of Severe Pre-Eclampsia
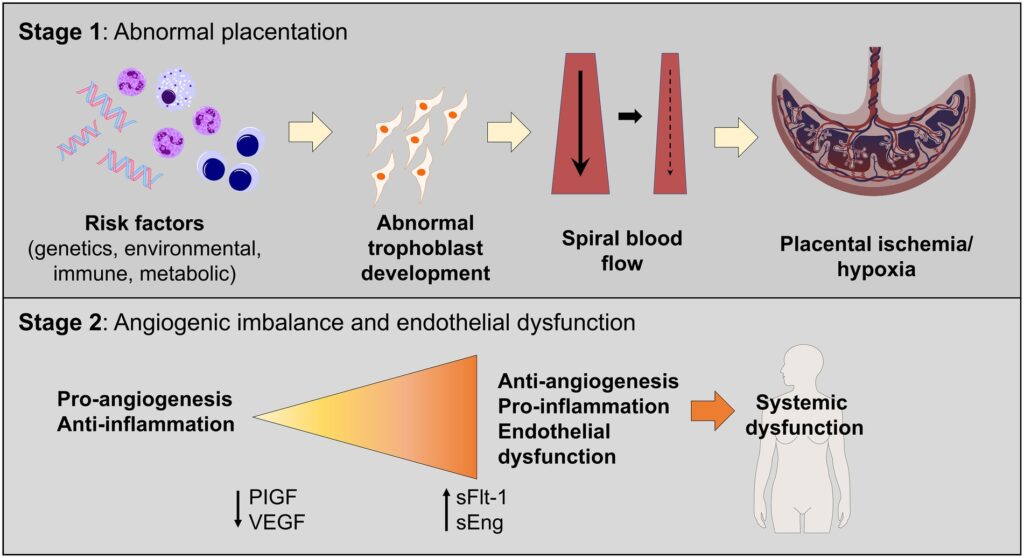
Severe pre-eclampsia stems from abnormal placentation. Inadequate remodeling of spiral arteries leads to placental ischemia, releasing antiangiogenic factors such as sFlt-1 and endoglin, which impair endothelial function. The result is systemic vasoconstriction, increased vascular permeability, and multi-organ damage.
Clinical Features and Presentation
- Severe headache
- Blurry vision or scotomata
- Nausea, vomiting, and epigastric pain
- Sudden weight gain due to fluid retention
- Reduced fetal movements
- Shortness of breath (from pulmonary edema)
Maternal and Fetal Complications
Maternal Risks
- Eclampsia (seizures)
- HELLP Syndrome (Hemolysis, Elevated Liver enzymes, Low Platelets)
- Acute renal failure
- Disseminated intravascular coagulation (DIC)
- Stroke or intracranial hemorrhage
Fetal Risks
- Intrauterine growth restriction (IUGR)
- Placental abruption
- Oligohydramnios
- Preterm birth
- Stillbirth
Risk Factors for Severe Pre-Eclampsia
- Primigravida
- Previous history of pre-eclampsia
- Multiple gestation
- Pre-existing hypertension or renal disease
- Diabetes mellitus
- Obesity
- Advanced maternal age (>35)
Diagnostic Workup and Monitoring Protocol
| Test | Purpose |
|---|---|
| Complete blood count | Platelets, hemoglobin levels |
| Liver function tests | AST, ALT for liver involvement |
| Renal panel | Creatinine, uric acid |
| Coagulation profile | PT, aPTT, fibrinogen |
| 24-hour urine collection or protein/creatinine ratio | Proteinuria quantification |
| Fetal ultrasound | Biophysical profile and growth |
| Non-stress test | Fetal well-being |
Evidence-Based Management of Severe Pre-Eclampsia
Hospitalization and Monitoring
All patients require immediate admission for continuous monitoring of:
- Blood pressure (every 15–30 minutes)
- Urine output (target >30 mL/hour)
- Fetal heart rate
- Neurological status
Antihypertensive Therapy
To prevent cerebrovascular accidents:
| Drug | Dose | Notes |
|---|---|---|
| Labetalol | 20–80 mg IV bolus | First-line |
| Hydralazine | 5–10 mg IV | Alternative |
| Nifedipine | 10 mg orally | Used if IV access delayed |
Goal: Maintain BP <160/110 mmHg without compromising placental perfusion.
Seizure Prophylaxis
Magnesium sulfate is the gold standard:
- Loading dose: 4–6 g IV over 20 minutes
- Maintenance: 1–2 g/hr infusion
Monitor: Reflexes, respiratory rate, and urine output to avoid toxicity.
Timing of Delivery
- ≥34 weeks: Prompt delivery recommended
- <34 weeks: Expectant management if stable, with corticosteroids (e.g., betamethasone) for fetal lung maturation
- Any gestational age: Immediate delivery if maternal or fetal condition deteriorates
Postpartum Considerations
- Close BP monitoring for at least 72 hours postpartum
- Antihypertensives may be continued or tapered
- Seizure risk persists up to 48 hours post-delivery
- Monitor for HELLP or DIC post-delivery
- Long-term cardiovascular follow-up due to increased lifetime risk of hypertension, stroke, and heart disease
Prevention Strategies and Long-Term Outlook
Preventive Interventions
- Low-dose aspirin (81–150 mg daily) starting at 12–16 weeks in high-risk women
- Calcium supplementation in women with low dietary intake
- Weight optimization before pregnancy
- Preconception counseling for high-risk patients
Prognosis
With prompt diagnosis and delivery, maternal mortality is significantly reduced. However, risks of future pre-eclampsia, chronic hypertension, and cardiovascular disease warrant long-term follow-up.
Severe pre-eclampsia demands urgent, multidisciplinary management to prevent devastating maternal and fetal complications. With vigilant monitoring, timely intervention, and appropriate delivery decisions, outcomes can be significantly optimized. Early identification of risk and postnatal care are crucial to reduce recurrence and safeguard long-term health.