Severe pain represents an intense, often debilitating sensory and emotional experience associated with actual or potential tissue damage. It may arise suddenly as acute pain or persist chronically for months or years. Whether linked to trauma, disease, surgery, or nerve dysfunction, its impact extends beyond physical distress, impairing mental well-being, functional capacity, and overall quality of life.
Types of Severe Pain Based on Pathophysiology
- Nociceptive Pain: From tissue injury—sharp, aching, or throbbing in nature
- Neuropathic Pain: From nerve damage—burning, shooting, or electric sensations
- Inflammatory Pain: Driven by immune-mediated tissue inflammation
- Functional Pain: Abnormal pain perception without evident tissue damage
Common Causes of Severe Pain
Post-Surgical Pain
Intense pain following major surgery, especially orthopedic, spinal, or thoracic procedures, can persist if not managed promptly.
Cancer-Related Pain
Infiltration of nerves, bones, or organs by malignant tumors leads to progressive, unrelenting pain often requiring specialized palliative care.
Musculoskeletal Disorders
- Osteoarthritis: Degenerative joint pain
- Disc herniation: Radicular nerve pain
- Complex regional pain syndrome (CRPS): Severe regional pain with autonomic changes
Neurological Conditions
- Diabetic neuropathy
- Postherpetic neuralgia
- Multiple sclerosis-related pain
Vascular and Ischemic Pain
- Peripheral arterial disease: Claudication
- Myocardial infarction: Crushing chest pain
- Ischemic bowel disease: Severe abdominal pain
Recognizing Symptoms and Pain Assessment
Clinical Characteristics
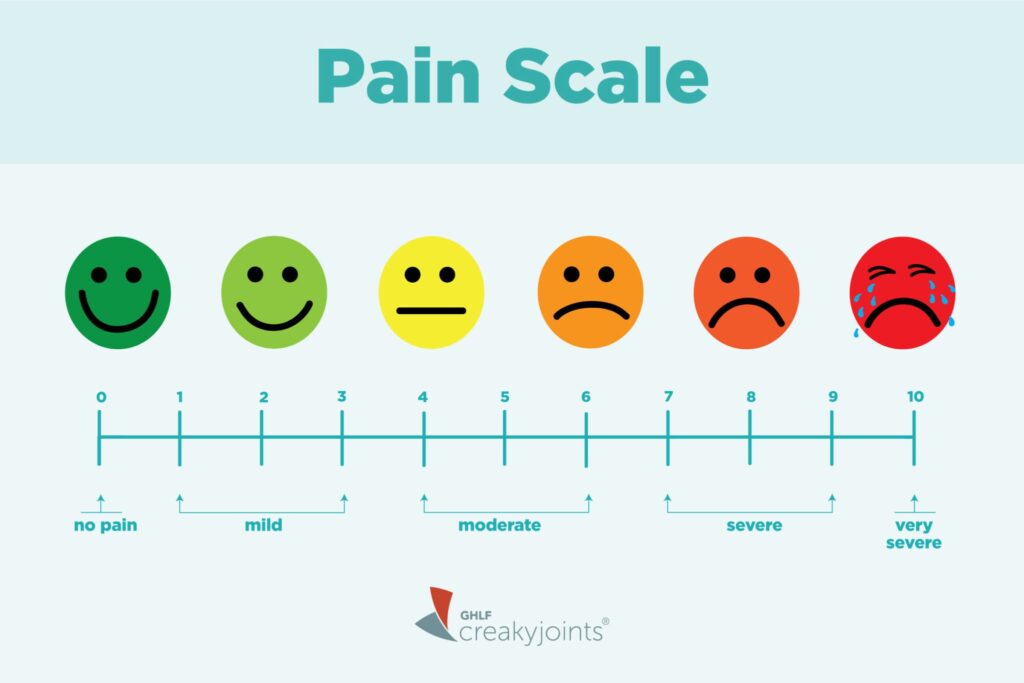
- Intensity: Often rated 7–10 on the numeric pain scale
- Duration: Acute (<3 months) or chronic (>3 months)
- Distribution: Localized, radicular, or diffuse
- Qualities: Burning, stabbing, throbbing, pressure-like
Tools for Objective Pain Evaluation
- Visual Analog Scale (VAS)
- Numeric Rating Scale (NRS)
- McGill Pain Questionnaire (MPQ)
- Brief Pain Inventory (BPI)
Diagnostic Approach for Severe Pain
Clinical Evaluation
- Detailed history of onset, location, and modifiers
- Physical and neurological examination for sensory deficits or motor impairment
Imaging Modalities
- MRI: For soft tissue, spine, or nerve compression
- CT scan: Useful in trauma or complex bony structures
- Ultrasound: For musculoskeletal and abdominal pain origins
Electrophysiological Studies
- Nerve conduction studies (NCS)
- Electromyography (EMG)
Laboratory Investigations
- Inflammatory markers: CRP, ESR
- Autoimmune screening: ANA, RF
- Metabolic panels: Vitamin B12, glucose levels for neuropathy
Comprehensive Pain Management Strategies
Pharmacologic Interventions
Non-Opioid Analgesics
- Acetaminophen: First-line for mild to moderate pain
- NSAIDs: Ibuprofen, naproxen for inflammatory causes
Opioid Therapy
Reserved for severe acute or cancer pain:
- Morphine, oxycodone, fentanyl
- Careful titration and monitoring to avoid dependence
Neuropathic Pain Agents
- Gabapentin, pregabalin: Calcium channel modulators
- Tricyclic antidepressants (TCAs): Amitriptyline
- SNRIs: Duloxetine
Interventional Pain Procedures
- Nerve blocks: Local anesthetics for targeted relief
- Epidural steroid injections: For radiculopathy
- Spinal cord stimulation: In refractory neuropathic pain
- Radiofrequency ablation: For facet-mediated joint pain
Psychological and Behavioral Therapies
- Cognitive-behavioral therapy (CBT)
- Mindfulness-based stress reduction
- Biofeedback and relaxation training
Physical and Rehabilitative Therapies
- Physiotherapy: Range-of-motion and strengthening
- TENS therapy: Transcutaneous electrical nerve stimulation
- Occupational therapy: Adaptive strategies for daily living
Special Considerations in Chronic Severe Pain
Opioid Stewardship and Monitoring
Chronic opioid use requires:
- Risk-benefit analysis
- Use of prescription monitoring programs (PMPs)
- Regular reassessment and dose tapering plans
Multidisciplinary Pain Clinics
Integrated teams offering:
- Pain specialists
- Psychologists
- Physical therapists
- Social workers
This coordinated approach enhances outcomes in complex chronic pain cases.
Preventing Progression and Improving Quality of Life
- Early intervention: Reduces the risk of chronic pain syndromes
- Regular follow-up: To adjust therapy and prevent relapse
- Patient education: Empowers individuals in self-management
- Lifestyle adjustments: Sleep hygiene, exercise, nutrition
Severe pain represents a multifactorial clinical challenge demanding timely diagnosis and a tailored, interdisciplinary treatment plan. Effective management hinges on a comprehensive understanding of its origin, accurate assessment, and the application of evidence-based therapies that target both physical and emotional dimensions. Our objective remains not only pain control but the restoration of function and dignity.