Severe hypotension refers to an abnormally low blood pressure that compromises the body’s ability to deliver adequate oxygen and nutrients to vital organs. It is typically defined as a systolic blood pressure below 90 mmHg or a mean arterial pressure (MAP) under 65 mmHg. This condition may rapidly progress to life-threatening shock if not promptly diagnosed and managed. Recognizing severe hypotension as a medical emergency is critical, particularly in trauma, sepsis, cardiac failure, or anaphylaxis.
Pathophysiology of Severe Hypotension
Severe hypotension arises when systemic vascular resistance or cardiac output drops significantly. The inability to maintain perfusion pressure leads to organ hypoxia and subsequent failure. Three primary mechanisms are involved:
- Hypovolemic shock: Due to significant blood or fluid loss
- Cardiogenic shock: Resulting from myocardial dysfunction
- Distributive shock: Caused by excessive vasodilation (e.g., sepsis or anaphylaxis)
Common Causes of Severe Hypotension
Medical and Surgical Emergencies
- Hemorrhagic trauma: Internal or external bleeding reducing blood volume
- Sepsis: Systemic inflammatory response causing vasodilation and capillary leak
- Myocardial infarction: Impaired ventricular function lowering cardiac output
- Pulmonary embolism: Obstruction impeding right heart output
- Anaphylaxis: Widespread vasodilation and plasma leakage
- Neurogenic shock: Loss of sympathetic vascular tone from spinal cord injury
Drug-Induced Hypotension
- Antihypertensives (e.g., ACE inhibitors, beta-blockers)
- Diuretics leading to hypovolemia
- Anesthetic agents reducing vascular tone
- Nitrates in excess
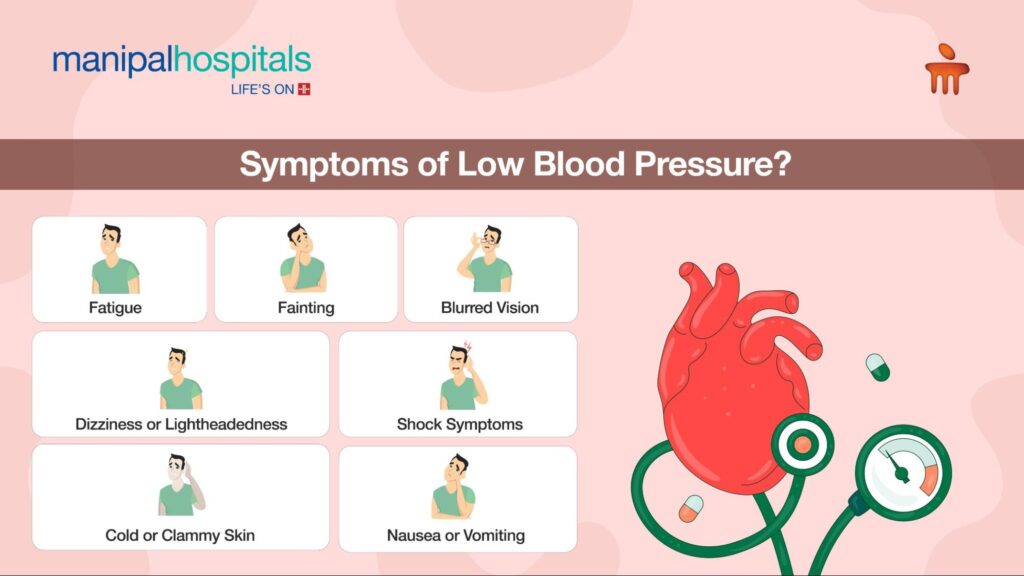
Recognizing the Symptoms of Severe Hypotension
The clinical presentation depends on the rate of blood pressure decline and the underlying cause. Key symptoms include:
- Dizziness or syncope
- Blurred vision or confusion
- Cold, clammy skin
- Tachycardia (early) or bradycardia (late)
- Oliguria or anuria
- Pallor or cyanosis
- Rapid, shallow breathing
- Chest pain or discomfort
In advanced cases, loss of consciousness or cardiac arrest may occur.
Diagnostic Approach to Severe Hypotension
Initial Clinical Assessment
- Measure blood pressure in both arms
- Assess level of consciousness and capillary refill
- Look for signs of bleeding, infection, or cardiac dysfunction
Key Diagnostic Tests
- Electrocardiogram (ECG): To evaluate cardiac rhythm and ischemia
- Serum lactate: Marker of tissue hypoperfusion
- Complete blood count (CBC): To detect anemia or infection
- Blood cultures: If sepsis is suspected
- Cardiac enzymes: In case of myocardial infarction
- Echocardiography: To assess ejection fraction and fluid status
- Chest X-ray or CT scan: To evaluate pulmonary or structural causes
Evidence-Based Treatment for Severe Hypotension
Immediate Resuscitation Measures
- Airway management: Ensure patency and adequate oxygenation
- Intravenous fluid resuscitation: Isotonic crystalloids like normal saline or lactated Ringer’s for hypovolemia
- Vasopressors: Initiated if hypotension persists after fluids
- Norepinephrine is the first-line agent
- Vasopressin or epinephrine may be added depending on etiology
- Inotropes: (e.g., dobutamine) used in cardiogenic shock
- Blood transfusion: Indicated in acute hemorrhage
Targeted Therapies
- Antibiotics for sepsis: Broad-spectrum within the first hour
- Antihistamines and epinephrine for anaphylaxis
- Pericardiocentesis or thrombolytics: In cardiac tamponade or massive PE
- Surgical intervention: For ongoing internal bleeding or vascular injury
Monitoring and Supportive Care
Hemodynamic Monitoring
- Continuous blood pressure monitoring via arterial line
- Central venous pressure (CVP) or pulmonary artery catheterization in critical care settings
Organ Support
- Mechanical ventilation in cases of respiratory compromise
- Renal replacement therapy for acute kidney injury
- Glucose and electrolyte correction
Complications of Severe Hypotension
- Multiple Organ Dysfunction Syndrome (MODS)
- Ischemic stroke
- Myocardial infarction
- Acute tubular necrosis and renal failure
- Metabolic acidosis
- Disseminated intravascular coagulation (DIC)
Prompt intervention is crucial to avoid irreversible cellular injury and fatal outcomes.
Prevention and Risk Reduction
Chronic Disease Management
- Control underlying conditions such as heart failure, diabetes, or infections
- Regular medication review to avoid overcorrection of blood pressure
Patient Education
- Instruct patients to rise slowly from lying or sitting positions to prevent orthostatic drops
- Adequate hydration and salt intake in predisposed individuals
- Compression stockings in cases of venous pooling
Special Populations and Considerations
Elderly Patients
Older adults are more susceptible due to impaired baroreceptor sensitivity and polypharmacy. Adjusting antihypertensive therapy and ensuring postural blood pressure measurements are essential.
Pregnancy
Severe hypotension during pregnancy, especially in the supine position, may indicate supine hypotensive syndrome. Left lateral positioning and fetal monitoring are indicated.
Severe hypotension is a critical condition requiring rapid assessment, precise diagnosis, and aggressive intervention. Whether due to hemorrhage, infection, cardiac compromise, or vasodilatory shock, management must be individualized based on the underlying etiology. Ongoing monitoring, hemodynamic support, and early definitive care remain the pillars of successful treatment and survival.

