Severe chronic pain, defined as pain persisting beyond three months and significantly impairing daily function, affects millions worldwide. For a subset of patients, non-opioid therapies prove insufficient, and long-term opioid treatment becomes medically necessary. In such cases, structured care, rigorous monitoring, and individualized strategies are essential to ensure effective pain relief while minimizing risk.
Indications for Long-Term Opioid Therapy in Chronic Pain Management
Long-term opioid therapy is considered appropriate for patients with:
- Intractable musculoskeletal disorders (e.g., failed back surgery syndrome)
- Neuropathic pain unresponsive to other agents
- Cancer-related pain in long-term survivors
- Rheumatologic conditions with persistent nociceptive and inflammatory pain
- Complex regional pain syndrome (CRPS) or advanced degenerative diseases
These conditions typically warrant opioid continuation when function is improved, side effects are tolerable, and alternatives have been exhausted.
Patient Selection and Risk Assessment
Comprehensive Pre-treatment Evaluation
Before initiating long-term opioid therapy, we conduct a multi-faceted assessment:
- Pain characteristics (location, duration, severity)
- Functional baseline and quality of life measures
- Mental health screening (depression, anxiety, substance use disorders)
- History of medication use and response to prior interventions
- Risk stratification for opioid misuse using validated tools such as the ORT (Opioid Risk Tool)
Principles of Safe Long-Term Opioid Prescribing
Individualized Dosing and Titration
- Start with lowest effective dose, adjusting gradually
- Use extended-release opioids for baseline control
- Employ immediate-release opioids sparingly for breakthrough pain
- Avoid exceeding 90 MME/day unless clearly justified
Opioid Rotation
When tolerance develops or side effects become problematic, opioid rotation—switching to a different opioid—can restore analgesic efficacy.
Equianalgesic Conversion Example
| Current Opioid | Dose (mg/day) | Target Opioid | Equivalent Dose (mg/day) |
|---|---|---|---|
| Morphine | 60 | Oxycodone | 40 |
| Fentanyl Patch | 25 mcg/hr | Morphine | 60–134 |
Note: Always apply a dose reduction factor when switching due to incomplete cross-tolerance.
Monitoring and Mitigation of Opioid Risks
Structured Follow-Up and Safety Measures
We implement standardized protocols to monitor therapy:
- Pain and function reassessments every 1–3 months
- Urine drug testing for adherence and illicit use
- Prescription drug monitoring program (PDMP) reviews
- Naloxone co-prescribing for patients at elevated overdose risk
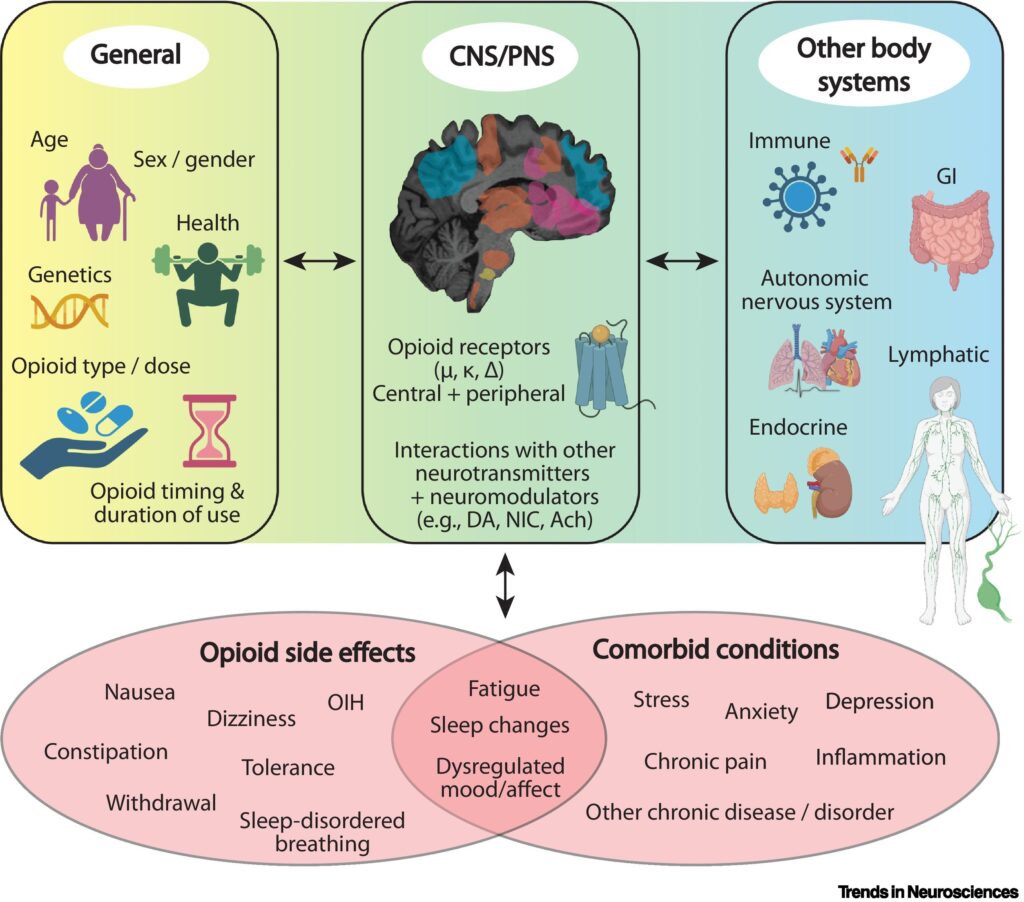
Adverse Effects and Management
| Side Effect | Management Strategy |
|---|---|
| Constipation | Laxatives, stool softeners, hydration |
| Sedation | Dose reduction, split dosing, stimulant use |
| Hormonal suppression | Monitor testosterone/cortisol, consider endocrinology referral |
| Opioid-induced hyperalgesia | Consider tapering or opioid rotation |
Integrating Multimodal Approaches for Optimal Pain Control
Long-term opioid use should always be part of a broader multimodal strategy:
- Adjuvant medications: Anticonvulsants, antidepressants
- Physical therapy: Enhances mobility, reduces stiffness
- Behavioral therapy: CBT, biofeedback for pain coping
- Interventional procedures: Nerve blocks, epidural injections
- Mind-body therapies: Yoga, meditation, mindfulness-based stress reduction
Tapering and Discontinuation Protocols
When to Consider Opioid Tapering
- Lack of functional improvement
- Adverse effects outweighing benefits
- Aberrant drug behaviors or suspected misuse
- Patient request
Tapering Guidelines
- Reduce dose by 5–10% every 2–4 weeks
- Provide psychological and pharmacologic support
- Monitor for withdrawal symptoms and pain flare-ups
- Offer non-opioid alternatives throughout the process
Ethical and Regulatory Considerations
Healthcare providers must balance ethical responsibility for pain relief with regulatory obligations to prevent misuse. Key frameworks include:
- CDC Guidelines for Prescribing Opioids
- FDA REMS Programs (Risk Evaluation and Mitigation Strategies)
- State medical board policies and opioid prescribing laws
We ensure full documentation of clinical rationale, goals, informed consent, and shared decision-making for long-term opioid treatment.
Future Directions in Chronic Pain and Opioid Research
Innovative approaches are reshaping chronic pain management:
- Peripheral nerve stimulation and neuromodulation as opioid-sparing strategies
- Gene therapy targeting pain receptors and inflammatory pathways
- Digital therapeutics incorporating virtual CBT and pain tracking apps
- Opioid vaccines under development to block drug effects and reduce addiction risk
Long-term opioid treatment for severe chronic pain is a necessary, life-improving intervention for select patients. A structured, risk-aware, and multidisciplinary model ensures safety, efficacy, and respect for the complexity of chronic pain. By integrating pharmacologic precision with functional goals and patient-centered care, we can achieve sustained relief without compromising accountability.