Severe chronic pain in children, particularly those who are opioid-tolerant, presents a complex and demanding clinical scenario. Defined as pain lasting more than three months, it significantly disrupts development, social function, education, and emotional well-being. In opioid-tolerant pediatric patients, typical analgesic strategies are insufficient, requiring tailored, closely monitored regimens.
Opioid Tolerance in Children: Definition and Clinical Relevance
Opioid tolerance occurs when sustained exposure to opioids results in diminished analgesic effects, requiring escalating doses to maintain pain relief. In pediatric patients, this often stems from long-term treatment of conditions such as:
- Cancer
- Sickle cell disease
- Complex regional pain syndrome (CRPS)
- Neuropathic disorders
- Post-surgical complications
Recognition of opioid tolerance is essential to adjust dosing appropriately and prevent both under-treatment and overdose.
Etiologies of Chronic Pain in Pediatric Patients Aged 11 and Older
| Condition | Description |
|---|---|
| Juvenile Idiopathic Arthritis | Chronic inflammation of joints causing pain and stiffness |
| Ehlers-Danlos Syndrome | Connective tissue disorder with joint pain and dislocations |
| Post-surgical Pain | Persistent pain following procedures such as spinal fusion or thoracotomy |
| Cancer-related Pain | Pain resulting from tumors or chemotherapy complications |
| Neuropathic Pain | Often due to nerve damage, infections, or autoimmune processes |
Comprehensive Pain Assessment in Opioid-Tolerant Pediatric Patients
Key Components of Evaluation
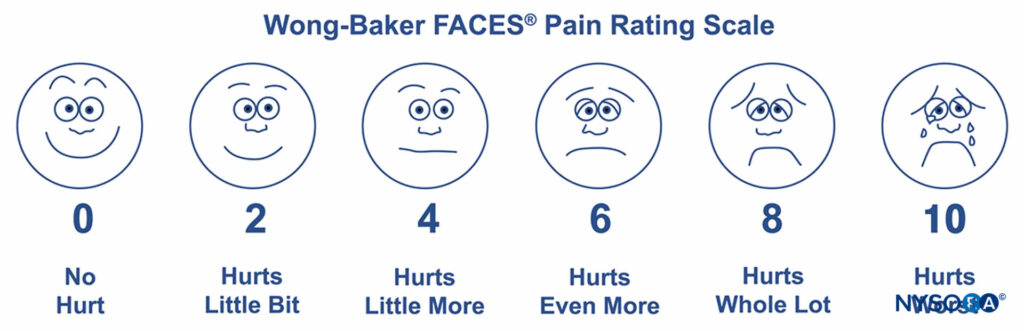
- Pain history including onset, location, intensity, and triggers
- Functional assessment focusing on mobility, sleep, schooling, and emotional status
- Medication review with special attention to previous opioid use, dose, and response
- Psychosocial screening for anxiety, depression, or PTSD
Individualized Pain Management Strategies
Pharmacologic Therapy in Opioid-Tolerant Pediatric Patients
Pain control in opioid-tolerant children necessitates the use of potent agents with adjusted dosages:
| Drug Class | Examples | Role in Treatment |
|---|---|---|
| Extended-release opioids | Morphine ER, Oxycodone ER | Baseline control for continuous pain |
| Short-acting opioids | Fentanyl, Hydromorphone | Rescue dosing for breakthrough pain |
| Adjuvants | Gabapentin, Duloxetine | Neuropathic and mixed pain modulation |
| Anti-inflammatory agents | Naproxen, Ibuprofen | Reduce inflammation and synergize analgesia |
Dosing Principles:
- Adjust based on weight, age, and degree of tolerance
- Employ equianalgesic conversion tables cautiously
- Monitor renal and hepatic function regularly
Safety Considerations and Risk Mitigation
Monitoring and Risk Management Plan
Essential Components:
- Continuous monitoring of sedation, respiratory status, and adverse effects
- Naloxone prescription for emergency use
- Scheduled follow-up visits to review functional outcomes and medication efficacy
- Urine drug screening when indicated
Non-Pharmacologic Interventions in Chronic Pediatric Pain
Psychological Therapies
- Cognitive Behavioral Therapy (CBT)
Alters pain perception and improves coping strategies. - Acceptance and Commitment Therapy (ACT)
Encourages behavioral flexibility and values-driven goals despite pain.
Physical Rehabilitation
- Customized physical therapy to restore mobility and reduce muscle tension
- Occupational therapy to enhance daily living function
- Graded exercise programs to reduce deconditioning
Complementary Techniques
- Biofeedback and guided imagery
- Acupuncture
- Music and art therapy to address emotional dimensions of pain
Role of Multidisciplinary Pain Teams
A multidisciplinary team is central to optimal outcomes:
- Pediatric pain specialists guide pharmacologic regimens
- Psychologists manage emotional and behavioral aspects
- Rehabilitation therapists restore physical function
- Social workers assist with family support and school reintegration
Transitioning to Adulthood and Chronic Pain Continuity
As opioid-tolerant pediatric patients approach adolescence and adulthood, structured transitional planning becomes essential. This includes:
- Identifying adult pain care providers
- Managing opioid tapering where feasible
- Educating patients on medication responsibility and safe use
- Preparing for college, employment, and independent living with chronic pain
Challenges in Management and Future Directions
Key Challenges
- Limited data on long-term opioid safety in children
- Risk of opioid-induced hyperalgesia and psychological dependency
- Stigma around pediatric opioid use
Emerging Therapies
- Cannabinoids: Under investigation for select pediatric pain conditions
- Neuromodulation: Spinal cord stimulation and transcranial magnetic stimulation
- Gene therapy: Promising in inherited pain disorders and neuropathic mechanisms
Managing severe chronic pain in opioid-tolerant pediatric patients aged 11 and older requires precision, compassion, and collaboration. Balancing effective analgesia with safety, function, and quality of life is paramount. A multidisciplinary, individualized approach anchored in continuous reassessment enables optimal outcomes for these vulnerable patients and their families.

