Severe chronic obstructive pulmonary disease (COPD) is a progressive, irreversible lung condition marked by persistent airflow limitation and respiratory symptoms. It results from chronic inflammatory responses to harmful particles or gases, most commonly from cigarette smoke. Severe COPD significantly impairs daily activities, quality of life, and increases the risk of life-threatening exacerbations.
COPD Pathophysiology and Disease Mechanism
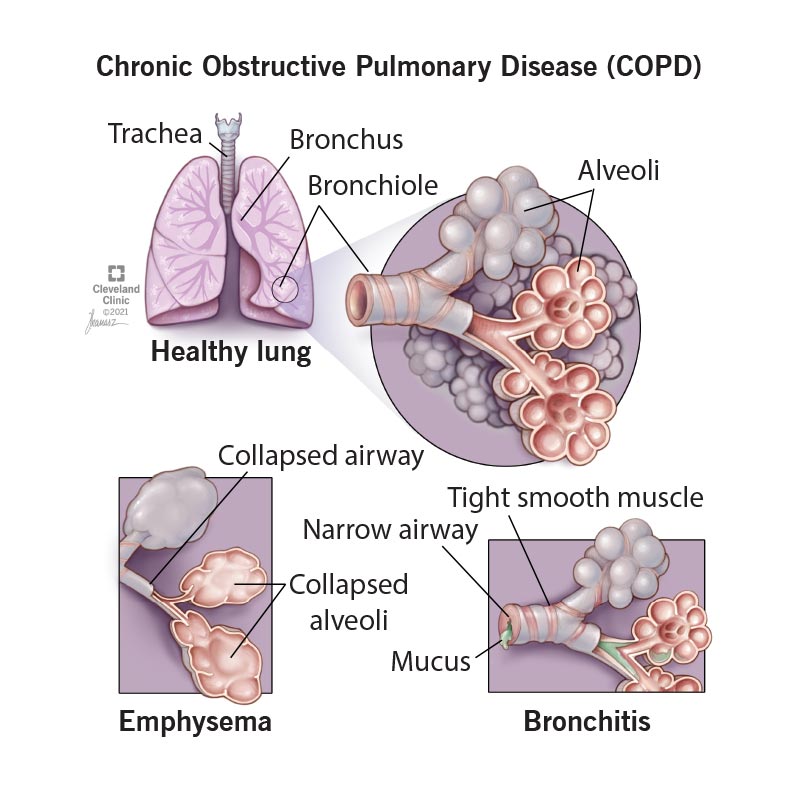
COPD encompasses two primary conditions:
- Chronic bronchitis – chronic inflammation of the bronchial tubes causing mucus hypersecretion
- Emphysema – destruction of alveolar walls leading to reduced gas exchange
These mechanisms contribute to airway obstruction, air trapping, and hyperinflation of the lungs.
GOLD Classification of COPD Severity
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) provides a standardized classification based on post-bronchodilator forced expiratory volume in one second (FEV₁):
| GOLD Stage | FEV₁ % Predicted | Severity Level |
|---|---|---|
| GOLD 1 | ≥80% | Mild |
| GOLD 2 | 50–79% | Moderate |
| GOLD 3 | 30–49% | Severe |
| GOLD 4 | <30% | Very Severe |
Severe COPD (GOLD 3) is characterized by marked airflow limitation, dyspnea during minimal exertion, frequent exacerbations, and reduced exercise tolerance.
Common Symptoms in Severe COPD
- Persistent cough with sputum
- Pronounced shortness of breath (especially during exertion)
- Wheezing and chest tightness
- Fatigue and reduced physical stamina
- Recurrent respiratory infections
- Weight loss and muscle wasting in advanced stages
Risk Factors Contributing to Severe COPD
Primary Risk Factors
- Cigarette smoking – the most significant contributor
- Long-term occupational exposure to dust, chemicals, and fumes
- Air pollution, especially in urban settings
- Genetic predisposition, such as alpha-1 antitrypsin deficiency
- Respiratory infections in early childhood
Diagnostic Evaluation of Severe COPD
Pulmonary Function Testing (PFT)
- Spirometry is the gold standard for diagnosing COPD.
- Key criteria: FEV₁/FVC < 0.70 post-bronchodilator confirms persistent airflow obstruction.
Imaging Studies
- Chest X-ray may show hyperinflation or flattened diaphragm.
- High-resolution CT (HRCT) detects emphysematous changes and rule out alternative diagnoses.
Laboratory Tests
- Arterial blood gases (ABG) in advanced stages to assess hypoxemia or hypercapnia.
- Alpha-1 antitrypsin level for early-onset or non-smoker COPD cases.
Medical Management of Severe Chronic Obstructive Pulmonary Disease
Pharmacologic Treatment
Bronchodilators
- Long-acting beta-agonists (LABAs) and long-acting muscarinic antagonists (LAMAs) are first-line.
- Combination inhalers (LABA/LAMA or LABA/ICS) improve symptoms and reduce exacerbations.
Inhaled Corticosteroids (ICS)
- Added in patients with frequent exacerbations or asthma-COPD overlap.
Phosphodiesterase-4 Inhibitors
- Roflumilast reduces inflammation and is indicated in severe COPD with chronic bronchitis.
Oxygen Therapy
- Indicated for patients with resting PaO₂ ≤ 55 mmHg or SaO₂ ≤ 88%
- Improves survival in hypoxemic COPD patients when used ≥15 hours/day
Vaccinations
- Influenza, pneumococcal, and COVID-19 vaccines are essential to prevent infections.
Non-Pharmacologic Therapies
Pulmonary Rehabilitation
- Structured exercise training, education, and psychological support
- Shown to improve quality of life and exercise capacity
Nutritional Support
- High-protein, energy-dense diet to counter cachexia
- Nutritional supplementation in underweight individuals
Breathing Techniques and Airway Clearance
- Pursed-lip breathing and diaphragmatic breathing
- Positive expiratory pressure devices for mucus clearance
Surgical and Interventional Approaches
Lung Volume Reduction Surgery (LVRS)
- Removal of diseased, non-functioning lung tissue to improve diaphragmatic mechanics
- Indicated in upper-lobe predominant emphysema
Bronchoscopic Lung Volume Reduction (BLVR)
- Less invasive alternative using endobronchial valves or coils
Lung Transplantation
- Considered for patients under 65 with very severe COPD, poor prognosis, and failure of other treatments
Managing Acute Exacerbations in Severe COPD
Exacerbations are defined as an acute worsening of respiratory symptoms requiring additional therapy.
Treatment Protocol
- Short-acting bronchodilators (SABAs) for immediate relief
- Systemic corticosteroids (e.g., prednisone 40 mg/day for 5 days)
- Antibiotics if signs of bacterial infection are present (e.g., purulent sputum)
- Non-invasive ventilation (NIV) in cases of respiratory acidosis
Prompt recognition and early intervention are crucial to reduce hospitalizations and mortality.
Complications of Severe COPD
- Respiratory failure
- Pulmonary hypertension leading to cor pulmonale
- Cardiac arrhythmias
- Osteoporosis due to systemic corticosteroid use
- Depression and anxiety
Prognosis and End-of-Life Considerations
Prognostic Indicators
- Frequency of exacerbations
- Rapid decline in FEV₁
- Hypoxemia and hypercapnia
- Body mass index (BMI) <21
- Exercise tolerance (6-minute walk test)
Palliative Care in End-Stage COPD
- Focus on symptom control (dyspnea, anxiety, fatigue)
- Advanced directives and end-of-life planning
- Hospice referral when life expectancy is ≤6 months
Severe chronic obstructive pulmonary disease represents a significant global health challenge, leading to functional decline, comorbidities, and mortality. Early recognition, adherence to evidence-based therapies, and integrated care models including pulmonary rehabilitation, nutritional support, and patient education are essential to managing the disease effectively. Advancements in interventional pulmonology and individualized therapy offer new hope for improving quality of life in affected individuals.

