Severe chronic neutropenia (SCN) is a rare hematologic disorder characterized by persistently low levels of neutrophils, a vital type of white blood cell essential for combating bacterial and fungal infections. Patients with SCN are predisposed to recurrent infections, often beginning in infancy or early childhood, and the condition can progress to severe complications, including bone marrow failure or leukemia. Prompt diagnosis, genetic evaluation, and sustained clinical management are crucial for long-term outcomes.
Understanding Neutropenia and Its Classification
What Is Neutropenia?
Neutropenia is defined by an abnormally low absolute neutrophil count (ANC), typically measured in cells per microliter (μL) of blood. Normal ANC ranges between 1,500 and 8,000/μL. Neutropenia is classified as:
- Mild: ANC 1,000–1,500/μL
- Moderate: ANC 500–1,000/μL
- Severe: ANC <500/μL
Chronic vs. Acute Neutropenia
- Acute neutropenia is transient and typically associated with infection or drug exposure.
- Chronic neutropenia persists for more than three months and often has genetic or autoimmune etiology.
Etiology of Severe Chronic Neutropenia
Congenital Forms
Congenital neutropenia arises from genetic mutations affecting neutrophil development:
- Severe congenital neutropenia (Kostmann syndrome): Mutations in ELANE, HAX1, G6PC3, or GFI1 genes disrupt myeloid differentiation.
- Cyclic neutropenia: Caused by ELANE mutations, it features periodic ANC fluctuations every 21 days.
- Shwachman-Diamond syndrome: Includes neutropenia with pancreatic insufficiency and skeletal abnormalities.
Acquired Causes
Although the focus is on congenital cases, acquired chronic neutropenia may result from:
- Autoimmune disorders (e.g., systemic lupus erythematosus)
- Drug-induced marrow suppression
- Chronic infections (e.g., HIV, tuberculosis)
- Myelodysplastic syndromes
Clinical Manifestations of SCN
Patients with severe chronic neutropenia often present with:
- Recurrent fevers
- Mouth ulcers and gingivitis
- Skin abscesses
- Pneumonia or otitis media
- Perirectal infections
- Delayed wound healing
Early identification of these signs, particularly in children with frequent infections, is key to early diagnosis.
Diagnostic Evaluation and Laboratory Testing
Hematologic Investigations
- Complete blood count (CBC) with differential reveals persistent ANC <500/μL.
- Bone marrow biopsy shows a maturation arrest of myeloid precursors at the promyelocyte or myelocyte stage.
Genetic Testing
Molecular analysis is essential for identifying gene mutations. Common testing panels include:
- ELANE, HAX1, G6PC3, CSF3R, SBDS, and GFI1
- Next-generation sequencing (NGS) expedites diagnosis and guides management.
Monitoring and Surveillance
- Serial CBCs over time to assess stability of neutropenia.
- ANC charting for detecting cyclic trends.
- Annual bone marrow exams may be warranted to monitor for clonal evolution or dysplasia.
Pathogenesis and Genetic Pathways
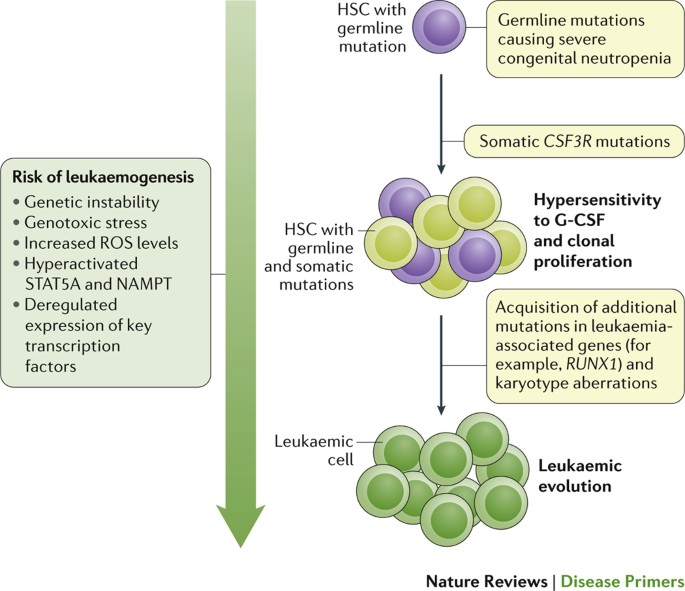
Severe congenital neutropenia results from defective neutrophil maturation due to mutations in genes regulating granulopoiesis.
- ELANE mutations cause accumulation of misfolded neutrophil elastase, triggering unfolded protein response and apoptosis.
- HAX1 mutations disrupt mitochondrial stability, impairing progenitor survival.
- G6PC3 affects energy metabolism in neutrophil precursors.
Management of Severe Chronic Neutropenia
First-Line Therapy: G-CSF
Granulocyte colony-stimulating factor (G-CSF) is the cornerstone of SCN treatment.
- Filgrastim administered subcutaneously
- Dose adjusted to maintain ANC >1,000/μL
- Reduces infection frequency and hospitalizations
Antibiotic Prophylaxis
Used in conjunction with G-CSF in high-risk patients:
- Trimethoprim-sulfamethoxazole (TMP-SMX) is commonly prescribed
- Empirical IV antibiotics for febrile neutropenia
Hematopoietic Stem Cell Transplant (HSCT)
Indicated in:
- G-CSF-resistant cases
- Development of myelodysplasia or leukemia
- Severe bone marrow dysfunction
Supportive Measures
- Strict oral hygiene
- Prompt wound care
- Vaccination updates, including pneumococcal and influenza vaccines
Complications and Long-Term Risks
Leukemic Transformation
- 10–20% of SCN patients may progress to acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS)
- CSF3R mutations frequently accompany leukemic evolution
- Requires vigilant long-term surveillance and early transplant consideration
Psychosocial Impact
Chronic illness in pediatric patients often entails:
- School absenteeism
- Anxiety related to recurrent infections
- Family stress from frequent medical care
Psychological support is a crucial component of comprehensive care.
Prognosis and Life Expectancy
With consistent G-CSF therapy and regular monitoring, many individuals with SCN can lead relatively normal lives. Early detection of complications and timely transplant when indicated significantly improve long-term outcomes.
Severe chronic neutropenia is a rare but potentially life-threatening hematologic disorder that demands early diagnosis, genetic insight, and ongoing clinical management. Advances in molecular genetics and targeted therapy, particularly G-CSF, have drastically improved patient survival and quality of life. A multidisciplinary approach involving hematologists, infectious disease specialists, and genetic counselors is essential for optimal care.