Severe adrenal insufficiency is a potentially life-threatening endocrine disorder resulting from inadequate production of cortisol and, in some cases, aldosterone by the adrenal glands. Cortisol plays a critical role in maintaining blood pressure, glucose metabolism, and immune regulation. Failure to promptly diagnose and treat this condition, especially during acute stress, can result in adrenal crisis—a medical emergency with high morbidity and mortality.
Understanding the Types of Adrenal Insufficiency
Primary Adrenal Insufficiency (Addison’s Disease)
This form arises from intrinsic dysfunction of the adrenal cortex, commonly due to autoimmune destruction, infections (e.g., tuberculosis), hemorrhage, or metastasis.
- Cortisol and aldosterone are both deficient.
- Elevated ACTH and hyperpigmentation are characteristic findings.
Secondary Adrenal Insufficiency
Occurs when the pituitary fails to produce adequate ACTH, most often due to exogenous steroid withdrawal or pituitary pathology.
- Aldosterone secretion is typically preserved.
- Electrolyte imbalance is less pronounced compared to primary insufficiency.
Tertiary Adrenal Insufficiency
Results from impaired hypothalamic CRH production, frequently due to chronic glucocorticoid therapy or hypothalamic tumors.
Pathophysiology: The Role of Cortisol and Aldosterone
Cortisol deficiency disrupts:
- Glucose regulation: leading to hypoglycemia
- Vascular tone maintenance: causing hypotension and shock
- Anti-inflammatory responses: increasing susceptibility to infections
Aldosterone deficiency (in primary insufficiency) results in:
- Sodium loss
- Hyperkalemia
- Hypovolemia
Clinical Presentation of Severe Adrenal Insufficiency
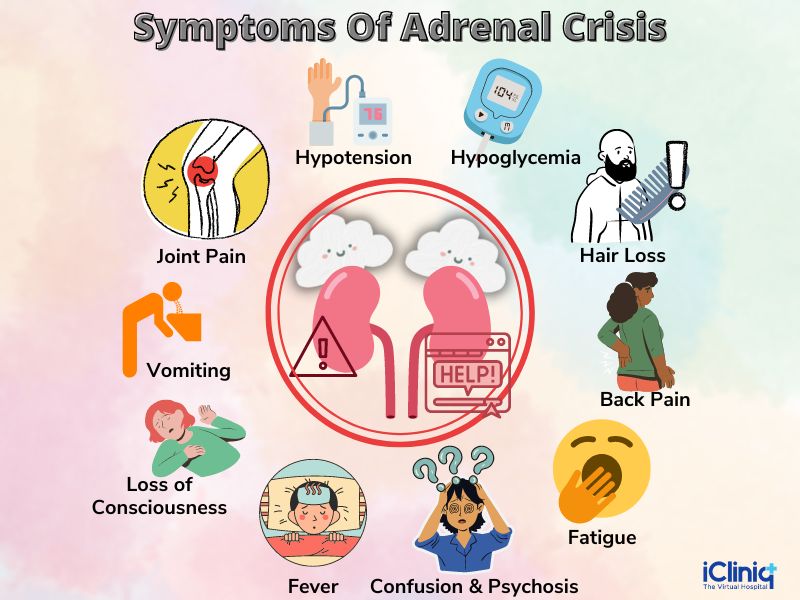
Chronic Symptoms
- Fatigue
- Weight loss
- Muscle weakness
- Nausea and abdominal pain
- Hyperpigmentation (primary type)
- Salt craving
Adrenal Crisis (Acute Presentation)
- Hypotension or shock
- Severe dehydration
- Hypoglycemia
- Confusion or coma
- Vomiting and abdominal pain
Prompt recognition of adrenal crisis is vital, particularly in undiagnosed patients under physiological stress (e.g., surgery, infection).
Diagnostic Approach to Adrenal Insufficiency
Baseline Investigations
- Morning serum cortisol (<3 µg/dL strongly suggests insufficiency)
- ACTH level (elevated in primary, low in secondary/tertiary)
- Electrolytes: hyponatremia, hyperkalemia
- Glucose: may be low
- Plasma renin activity and aldosterone (in primary)
ACTH Stimulation Test
- Synthetic ACTH (cosyntropin) is administered.
- Normal response: cortisol >18–20 µg/dL within 30–60 minutes.
- Blunted response indicates adrenal insufficiency.
Imaging and Additional Diagnostics
- CT scan of adrenal glands: useful in primary cases to assess for hemorrhage, tumors, or calcifications
- MRI of pituitary and hypothalamus: indicated in suspected secondary or tertiary insufficiency
- Autoantibody testing: 21-hydroxylase antibodies confirm autoimmune Addison’s disease
Emergency Management of Adrenal Crisis
Immediate steps:
- IV Hydrocortisone 100 mg bolus, followed by continuous infusion or 6-hourly doses.
- Rapid IV fluid resuscitation with 0.9% saline (1–3 L within first few hours).
- Correct hypoglycemia with dextrose infusion.
- Electrolyte monitoring and correction (especially potassium).
Failure to promptly administer corticosteroids is a common cause of fatality. Patients with known adrenal insufficiency must carry emergency identification and injectable hydrocortisone kits.
Long-Term Treatment and Maintenance Therapy
Glucocorticoid Replacement
- Hydrocortisone (15–25 mg/day) divided into 2–3 doses
- Alternatives: prednisone, dexamethasone (less physiologic)
Mineralocorticoid Replacement (Primary Only)
- Fludrocortisone acetate (0.05–0.2 mg daily)
- Titrated based on blood pressure, plasma renin, and electrolytes
Stress Dosing Protocols
Patients must increase glucocorticoid doses during illness, trauma, or surgery:
- Minor stress: double oral dose
- Major stress: IV hydrocortisone as in adrenal crisis
Monitoring and Follow-Up
- Routine assessment of BP, weight, fatigue, and electrolyte balance
- Regular renin and ACTH levels in primary insufficiency
- Bone density monitoring with long-term glucocorticoid use
- Education on stress dosing and emergency self-injection
Prevention of Adrenal Crisis
- Educate all patients and caregivers on emergency protocols.
- Provide medical alert bracelets and steroid emergency cards.
- Avoid abrupt discontinuation of corticosteroids.
- Initiate proper tapering schedules after long-term steroid therapy.
Severe adrenal insufficiency, whether primary, secondary, or tertiary, poses significant clinical risk, especially during physiological stress. Accurate diagnosis, prompt initiation of glucocorticoid therapy, and proper patient education are essential to reduce morbidity and prevent adrenal crises. Lifelong monitoring and individualized therapy ensure optimal patient outcomes and quality of life.

