Serratia urinary tract infections (UTIs) are uncommon but clinically significant infections caused primarily by Serratia marcescens, a gram-negative, facultative anaerobic bacillus. Most cases occur in healthcare settings and are often associated with indwelling urinary catheters or instrumentation. Due to Serratia’s intrinsic resistance to multiple antibiotics and its potential to cause persistent and recurrent infections, prompt diagnosis and appropriate management are essential.
Pathogenesis of Serratia Urinary Tract Infections
Serratia species, particularly S. marcescens, colonize moist environments and medical equipment. Invasive urinary procedures and compromised host immunity facilitate bacterial entry and proliferation in the urinary tract.
Risk Factors for Serratia UTIs
- Long-term indwelling urinary catheters
- Urological surgeries or instrumentation
- Immunocompromised states (e.g., diabetes, transplant patients)
- Prolonged antibiotic use
- Hospitalization, especially in ICUs
- Underlying urinary tract abnormalities or obstructions
Clinical Manifestations of Serratia UTIs
Lower Urinary Tract Symptoms (Cystitis)
- Dysuria (painful urination)
- Urinary frequency and urgency
- Suprapubic discomfort
- Cloudy or foul-smelling urine
- Hematuria (blood in urine)
Upper Urinary Tract Symptoms (Pyelonephritis)
- Flank pain and tenderness
- High-grade fever and chills
- Nausea and vomiting
- Malaise and systemic symptoms
Complicated Cases
- Urosepsis with hypotension and altered mental status
- Recurrent or relapsing infections despite antibiotic therapy
Diagnostic Evaluation
Laboratory Testing
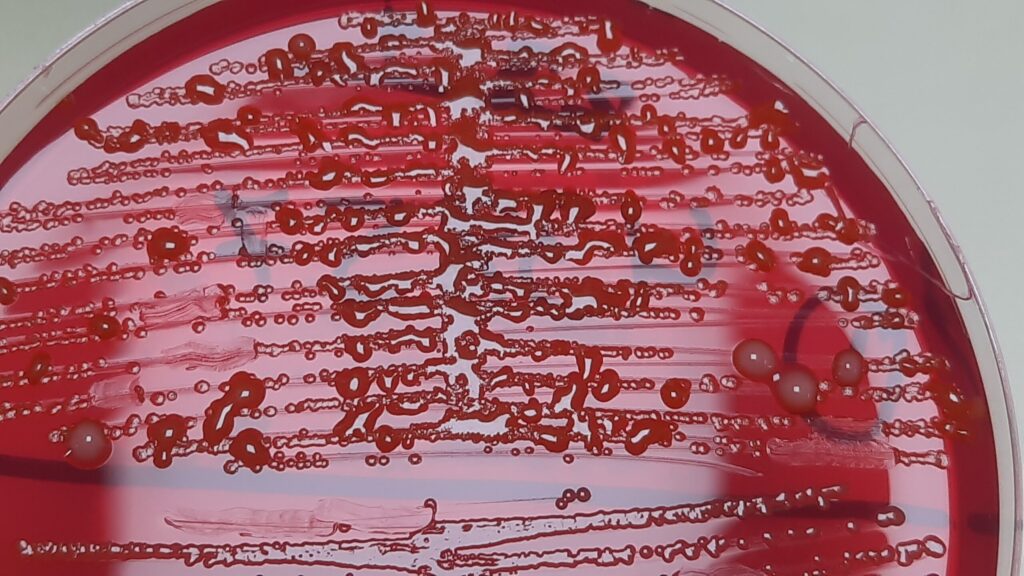
- Urinalysis: Presence of leukocyte esterase, nitrites, pyuria, and hematuria
- Urine culture: Growth of S. marcescens with quantification of colony-forming units
- Blood cultures: For suspected pyelonephritis or systemic involvement
Imaging
- Ultrasound or CT scan: Evaluation for obstructive uropathy, abscesses, or structural anomalies
Antimicrobial Susceptibility Testing
Due to Serratia’s resistance mechanisms (including AmpC β-lactamase), sensitivity testing is vital for effective treatment planning.
Treatment Strategies for Serratia Urinary Tract Infections
Empiric Therapy
Initiate broad-spectrum antibiotics pending culture results, particularly in severe infections:
- Carbapenems (e.g., meropenem or imipenem) for high-risk or hospitalized patients
- Fourth-generation cephalosporins (e.g., cefepime)
- Fluoroquinolones (e.g., ciprofloxacin or levofloxacin), if local resistance rates allow
Definitive Therapy
Tailor treatment based on susceptibility results:
- Ciprofloxacin (oral or IV)
- Trimethoprim-sulfamethoxazole (TMP-SMX)
- Aminoglycosides (e.g., gentamicin or amikacin, usually in combination therapy)
- Piperacillin-tazobactam, if susceptible
Duration of Therapy
- Uncomplicated UTI: 7–10 days
- Complicated UTI or pyelonephritis: 10–14 days
- Catheter-associated UTI (CAUTI): 10–21 days depending on severity and source control
Catheter-Associated Serratia UTIs (CAUTIs)
Serratia UTIs are often linked to long-term catheterization. Prevention and management include:
- Regular catheter care and early removal when feasible
- Use of closed drainage systems
- Replacing the catheter before obtaining culture samples
- Ensuring aseptic technique during insertion and maintenance
Resistance Mechanisms in Serratia Marcescens
Serratia exhibits intrinsic and acquired resistance due to:
- AmpC β-lactamase production: Confers resistance to penicillins and early cephalosporins
- Efflux pumps and porin mutations
- Biofilm formation: Enhances persistence on urinary catheters and surfaces
Avoid empiric use of ampicillin, amoxicillin-clavulanate, and first- or second-generation cephalosporins.
Prevention of Serratia UTIs
In Healthcare Settings
- Adherence to strict hand hygiene and infection control practices
- Routine surveillance cultures in high-risk units
- Periodic staff training on aseptic catheter insertion
In At-Risk Patients
- Avoid unnecessary catheterization
- Promote adequate hydration and bladder emptying
- Monitor closely for early signs of infection
Prognosis and Outcomes
Favorable Prognosis
- Early diagnosis and appropriate therapy generally result in recovery
- Proper catheter management reduces recurrence risk
Poor Prognostic Indicators
- Delayed treatment initiation
- Multidrug-resistant Serratia strains
- Immunosuppression or structural urological anomalies
Serratia urinary tract infections, while infrequent, represent a serious challenge due to their association with healthcare interventions and multidrug resistance. Accurate diagnosis, prompt susceptibility-guided treatment, and adherence to preventive strategies are essential in managing and reducing the burden of Serratia UTIs.

