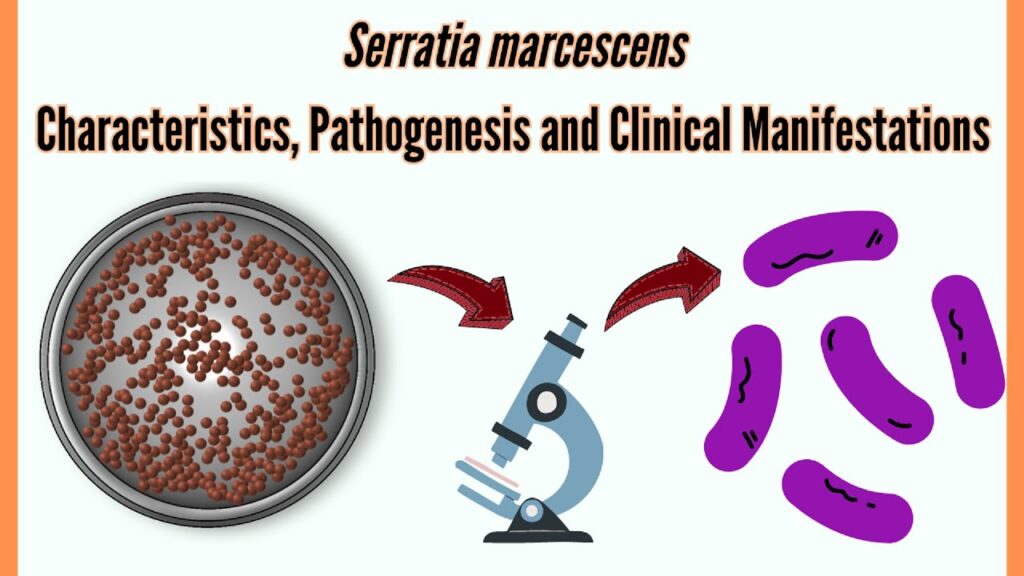
Serratia pneumonia is an uncommon but clinically significant pulmonary infection caused predominantly by Serratia marcescens, a facultative gram-negative bacillus. Although rare in healthy individuals, it poses a considerable threat in hospitalized or immunocompromised patients due to its inherent resistance to multiple antibiotics and association with ventilator-associated pneumonia (VAP) and healthcare-associated pneumonia (HCAP).
Pathophysiology and Transmission
Serratia marcescens colonizes moist hospital environments, including respiratory equipment, intravenous solutions, and catheters. Pneumonia results from direct aspiration, hematogenous dissemination, or mechanical ventilation-associated colonization.
Risk Factors for Serratia Pneumonia
- Prolonged hospitalization
- Mechanical ventilation
- Chronic lung disease (e.g., COPD)
- Recent antibiotic therapy
- Immunosuppression (e.g., transplant recipients, chemotherapy)
- Intensive care unit (ICU) admission
- Invasive medical devices (e.g., endotracheal tubes)
Clinical Presentation of Serratia Pneumonia
Respiratory Symptoms
- Productive cough with purulent or blood-tinged sputum
- Dyspnea and chest discomfort
- Fever with chills
- Tachypnea and hypoxia
Systemic Manifestations
- Sepsis or septic shock in severe cases
- Altered mental status in elderly or critically ill patients
- Respiratory failure requiring intubation
Diagnostic Evaluation
Laboratory Investigations
- Complete blood count (CBC): Leukocytosis with neutrophilia
- Procalcitonin and CRP: Elevated markers indicating bacterial infection
- Arterial blood gas (ABG): Hypoxemia in advanced disease
Microbiological Confirmation
- Sputum culture or bronchoalveolar lavage (BAL): Isolation of Serratia marcescens
- Blood cultures: Essential in systemic involvement
- Antibiotic susceptibility testing: Crucial due to resistance mechanisms (e.g., AmpC beta-lactamase)
Radiographic Imaging
- Chest X-ray or CT scan: Shows lobar consolidation, cavitation, or bilateral infiltrates typical of gram-negative pneumonia
Antimicrobial Therapy for Serratia Pneumonia
Due to high rates of resistance, empirical therapy should be adjusted based on local antibiograms and susceptibility profiles.
Empiric Treatment Options
- Cefepime or ceftazidime (4th-generation cephalosporins)
- Meropenem or imipenem (carbapenems)
- Levofloxacin or ciprofloxacin (fluoroquinolones)
Targeted Therapy
Once culture sensitivity is known, tailor treatment using:
- Ciprofloxacin (oral or IV for susceptible strains)
- Trimethoprim-sulfamethoxazole (when carbapenem-sparing is desired)
- Piperacillin-tazobactam (for non-resistant strains)
Avoid ampicillin, amoxicillin, and early-generation cephalosporins due to intrinsic resistance.
Duration of Therapy
- Uncomplicated cases: 10–14 days
- Complicated or ventilator-associated cases: Up to 21 days
Management in ICU and Ventilator Settings
Ventilator-Associated Serratia Pneumonia
- Elevate head of bed to reduce aspiration risk
- Regular oral hygiene with chlorhexidine
- Subglottic suctioning to minimize secretion accumulation
- Strict ventilator circuit maintenance and sterilization
Supportive Care Measures
- Oxygen supplementation or mechanical ventilation
- Intravenous fluids and vasopressors if septic shock is present
- Nutritional support in prolonged illness
Complications and Prognosis
Potential Complications
- Lung abscess
- Empyema (purulent pleural effusion)
- Bacteremia and septic shock
- Acute respiratory distress syndrome (ARDS)
- Multidrug-resistant recurrence
Prognostic Indicators
- Early antimicrobial intervention improves survival
- ICU-acquired infections have poorer outcomes
- Immunocompromised patients are at higher risk of mortality
Infection Control and Prevention Strategies
Hospital Protocols
- Enforce strict hand hygiene and PPE use
- Decontamination of respiratory and suction equipment
- Isolation of infected patients to prevent cross-transmission
- Judicious use of broad-spectrum antibiotics to limit resistance emergence
Preventive Measures in At-Risk Populations
- Minimize unnecessary intubation
- Regular surveillance cultures in ICU settings
- Prompt removal of unnecessary catheters or tubes
Serratia pneumonia, though rare, demands clinical attention due to its association with hospital-acquired infections and multidrug resistance. High clinical suspicion, timely diagnostics, and targeted antimicrobial therapy are essential for favorable outcomes. Strict adherence to infection control practices remains critical in preventing outbreaks in healthcare settings.