Serratia osteomyelitis is an uncommon but severe bone infection caused predominantly by Serratia marcescens, a gram-negative facultative anaerobic bacillus. While S. marcescens is more commonly associated with urinary tract and bloodstream infections, its involvement in osteomyelitis typically reflects nosocomial transmission, often linked to surgical interventions, orthopedic implants, or immunocompromised conditions.
The infection poses a substantial challenge due to delayed diagnosis, inherent antibiotic resistance, and its predilection for chronicity if inadequately treated.
Pathophysiology of Serratia-Induced Bone Infections
Mechanism of Bone Invasion
The bacterium may reach the bone tissue through:
- Hematogenous spread from distant sites of infection
- Direct inoculation during surgical procedures or trauma
- Contiguous spread from adjacent soft tissue infections
Upon colonization, Serratia marcescens produces biofilms on bone surfaces and prosthetic materials, making eradication difficult and facilitating resistance to antimicrobial agents.
Risk Factors for Serratia Osteomyelitis
- Recent orthopedic or spinal surgery
- Presence of bone implants or prosthetic joints
- Open fractures or bone trauma
- Immunosuppression (e.g., chemotherapy, HIV)
- Intravenous drug use
- Prolonged hospitalization or ICU stay
- Existing Serratia infections (e.g., urinary tract, bloodstream)
Clinical Presentation of Serratia Osteomyelitis
Localized Symptoms
- Persistent bone pain
- Localized swelling or redness
- Warmth over the affected area
- Limited range of motion in adjacent joints
- Formation of draining sinus tracts in chronic cases
Systemic Features
- Fever and chills
- Malaise
- Elevated inflammatory markers (CRP, ESR)
Diagnostic Approach
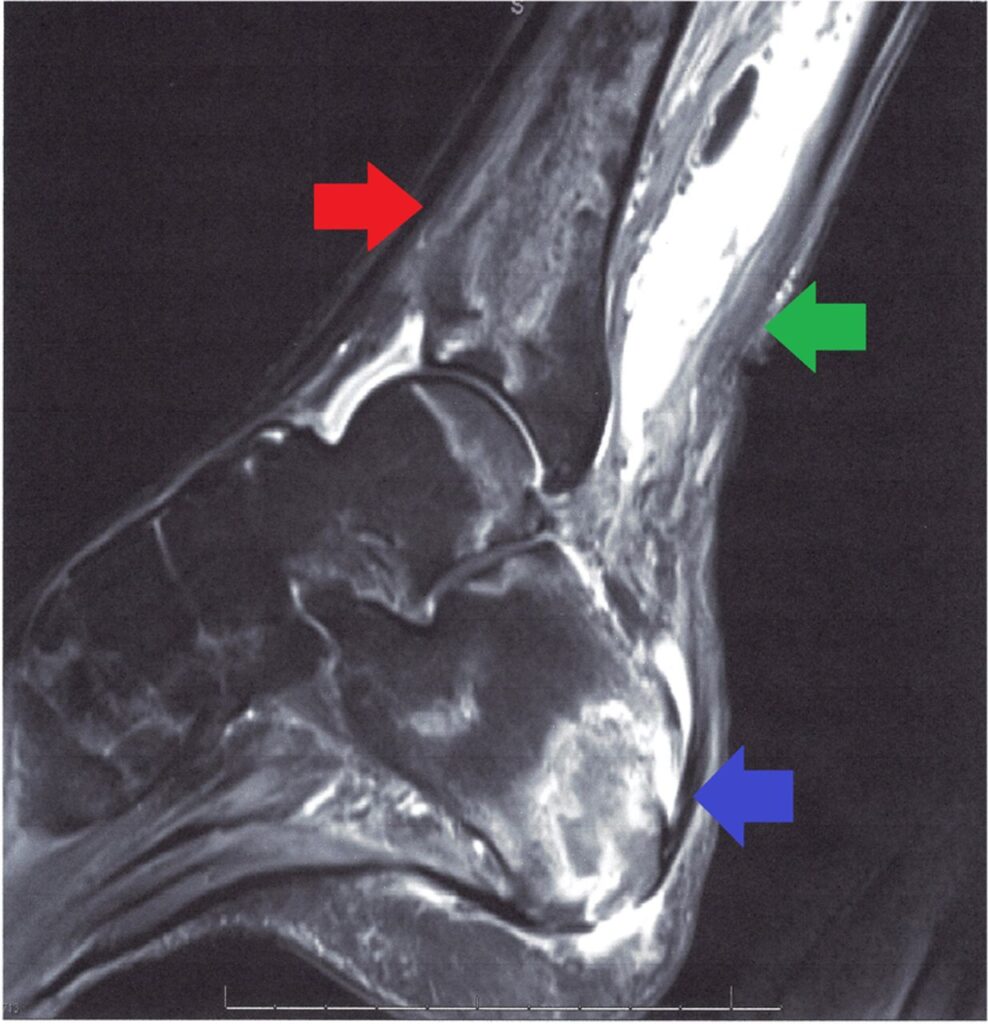
Imaging Studies
- X-rays may show lytic lesions or periosteal elevation in advanced stages
- MRI provides superior detail, identifying early marrow involvement and soft tissue spread
- CT scan aids in detecting bone sequestra and guiding surgical planning
Microbiological and Laboratory Tests
- Blood cultures to identify systemic dissemination
- Bone biopsy or aspirate for definitive diagnosis via culture and sensitivity
- CBC and inflammatory markers (WBC count, ESR, CRP) to evaluate systemic inflammation
Antimicrobial Therapy
Empiric Treatment
Initial broad-spectrum coverage is critical, often incorporating:
- Carbapenems (e.g., meropenem) for resistant gram-negative organisms
- Aminoglycosides (e.g., amikacin) for synergy
- Fluoroquinolones (e.g., ciprofloxacin) due to bone penetration and Serratia activity
Targeted Antibiotic Therapy
Once susceptibilities are known, therapy should be narrowed. Serratia marcescens is commonly resistant to ampicillin, first-generation cephalosporins, and may produce inducible AmpC beta-lactamases. Effective agents often include:
- Cefepime
- Meropenem
- Ciprofloxacin
- Trimethoprim-sulfamethoxazole
Surgical Management
Surgical intervention is often necessary for source control, particularly in chronic or refractory cases.
Indications for Surgery
- Failure of medical therapy
- Extensive bone necrosis or abscess formation
- Infected hardware or prosthesis
- Draining sinus tracts
Surgical Options
- Debridement of necrotic bone and soft tissue
- Removal of infected implants
- Bone grafting for reconstruction
- Long-term wound drainage management
Duration of Therapy and Follow-Up
- Intravenous antibiotics for 4 to 6 weeks, followed by oral therapy for select cases
- Close clinical and radiological monitoring during and after treatment
- Repeat imaging may be required to confirm resolution
Complications of Serratia Osteomyelitis
- Chronic osteomyelitis with persistent drainage
- Pathologic fractures
- Sepsis and systemic dissemination
- Joint involvement or septic arthritis
- Need for limb amputation in extreme cases
Prevention and Infection Control Measures
Hospital and Surgical Protocols
- Strict aseptic technique during surgery
- Proper sterilization of orthopedic instruments
- Limiting the use of indwelling devices unless absolutely necessary
Patient-Centered Strategies
- Prompt treatment of primary infections
- Regular follow-up in high-risk patients
- Early removal of orthopedic implants when infection is suspected
Prognosis
The prognosis of Serratia osteomyelitis depends on early recognition, pathogen susceptibility, and adequacy of both medical and surgical management. With appropriate therapy, many patients achieve resolution, though chronic infection and relapse remain concerns.
Serratia osteomyelitis, though rare, represents a serious threat to musculoskeletal integrity, particularly in hospital settings. Its management requires an integrated approach, including precise diagnosis, aggressive antibiotic therapy, and often surgical debridement. Ongoing surveillance and infection control are essential to prevent recurrence and reduce incidence.