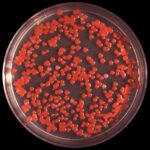
Serratia marcescens, a gram-negative bacillus from the Enterobacteriaceae family, is a rare but serious cause of septic arthritis, especially in immunocompromised hosts and patients with prosthetic joints. While more commonly implicated in urinary and respiratory infections, its ability to colonize orthopedic hardware and synovial tissue makes it a formidable pathogen in joint infections.
Complications such as biofilm formation, antimicrobial resistance, and delayed diagnosis necessitate aggressive and multidisciplinary management to preserve joint integrity and prevent systemic spread.

Risk Factors and Routes of Infection
Serratia joint infections typically occur through hematogenous spread, direct inoculation during surgery, or contiguous extension from adjacent infected tissues.
High-Risk Populations:
- Patients with prosthetic joints or orthopedic implants
- Individuals with recent joint injections or arthroscopy
- Immunocompromised patients (e.g., transplant recipients, diabetics)
- Hemodialysis patients with vascular access
- Injection drug users
- Patients in intensive care units or undergoing prolonged hospitalization
Clinical Features of Serratia Joint Infection
The presentation of Serratia-induced septic arthritis may mimic other bacterial or inflammatory arthropathies but often progresses more insidiously.
Common Symptoms:
- Acute or subacute monoarticular joint pain and swelling
- Restricted range of motion
- Fever, chills, and malaise (may be absent in immunosuppressed)
- Erythema and warmth over the joint
- In prosthetic joint infections: persistent pain or instability without overt systemic signs
The knee is most frequently involved, followed by hips, shoulders, and wrists.
Diagnostic Evaluation and Microbiological Confirmation
Prompt diagnosis is essential to initiate targeted therapy and prevent irreversible joint destruction.
Stepwise Diagnostic Approach:
- Synovial fluid aspiration
- Gram stain and culture
- White blood cell count (>50,000/mm³ with neutrophilic predominance)
- Crystal analysis to rule out gout or pseudogout
- Blood cultures
- Positive in hematogenous spread
- Imaging Studies
- X-ray: May show joint effusion or late-stage erosions
- Ultrasound: Identifies effusions for guided aspiration
- MRI or CT: Useful in deep-seated joints or prosthetic infection
- Tissue biopsy or periprosthetic tissue culture may be necessary in prosthetic joint infections or culture-negative cases.
Antimicrobial Resistance and Serratia Pathogenesis in Joints
Serratia marcescens possesses notable resistance mechanisms, contributing to the complexity of its eradication from joint spaces.
Key Resistance Mechanisms:
- AmpC β-lactamase production
- Extended-spectrum β-lactamases (ESBLs)
- Biofilm formation on synovium and prosthetic materials
- Efflux pumps and porin mutations
As a result, Serratia demonstrates intrinsic resistance to ampicillin, first-generation cephalosporins, and macrolides, and often shows multidrug resistance in hospital settings.
Definitive Antimicrobial Therapy for Serratia Joint Infection
Treatment must be culture-guided and may require prolonged intravenous antibiotics, especially in prosthetic joint infections.
Empiric Therapy (modified after susceptibility results):
- Carbapenems (meropenem, ertapenem) for resistant strains
- Fourth-generation cephalosporins (cefepime)
- Fluoroquinolones (ciprofloxacin, levofloxacin) if susceptible
- Aminoglycosides (amikacin, gentamicin) may be used synergistically
Duration of Therapy:
- Native joint infections: 3–4 weeks of IV antibiotics
- Prosthetic joint infections: 4–6 weeks of IV antibiotics, possibly followed by oral suppression depending on surgical outcome
Surgical Management of Serratia-Induced Septic Arthritis
Medical therapy alone is often insufficient in clearing Serratia joint infections due to biofilm persistence and structural damage.
Surgical Interventions:
- Arthroscopic or open joint drainage in native joints
- Debridement with implant retention (DAIR) in early prosthetic infections
- One-stage or two-stage prosthesis exchange in chronic infections
- Joint resection arthroplasty in non-salvageable cases
Complications of Serratia Joint Infection
Failure to initiate timely and appropriate management can result in significant morbidity.
Potential Complications:
- Joint destruction and deformity
- Chronic osteomyelitis
- Sepsis or bacteremia
- Functional impairment or disability
- Reinfection or treatment failure
Prosthetic joint infections are particularly prone to relapse if not adequately addressed surgically.
Prevention and Infection Control Strategies
Given the nosocomial origin of most Serratia joint infections, strict infection control protocols are imperative in hospital and surgical settings.
Preventive Measures:
- Aseptic surgical technique
- Perioperative antibiotic prophylaxis
- Sterile handling of joint injections
- Surveillance cultures in high-risk units
- Prompt treatment of primary infections to avoid hematogenous spread
Serratia Joint Infection in Immunocompromised Hosts
Patients with immune dysfunction present diagnostic and therapeutic challenges due to atypical symptoms, increased susceptibility, and poorer outcomes.
Special Considerations:
- Broader empiric antimicrobial coverage
- Extended duration of therapy
- Close monitoring for systemic dissemination
- Multidisciplinary management including rheumatology, infectious disease, and orthopedic surgery
Serratia joint infection represents a rare but aggressive form of septic arthritis requiring swift, multidisciplinary intervention. The pathogen’s capacity for resistance, biofilm formation, and nosocomial transmission elevates the complexity of treatment. Early recognition, targeted antimicrobial therapy, and timely surgical management are crucial for preserving joint function and preventing life-threatening complications. Ongoing vigilance and stringent infection control practices remain key to reducing the incidence and burden of Serratia-associated joint infections.