Serratia marcescens, a gram-negative, opportunistic bacillus from the Enterobacteriaceae family, is an emerging pathogen in complicated urinary tract infections (UTIs). These infections often arise in healthcare settings, especially in patients with urinary catheters, structural urologic abnormalities, or immunosuppressive conditions. Due to intrinsic and acquired resistance mechanisms, managing a Serratia complicated UTI requires a precise and evidence-based clinical approach.
Etiology and Pathogenesis of Serratia in Complicated UTIs
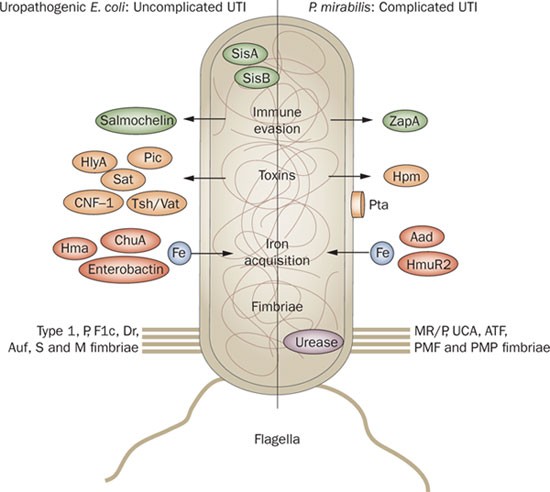
Serratia marcescens colonizes the urinary tract by adhering to uroepithelial cells and forming biofilms, particularly on indwelling devices. Its ability to produce β-lactamases and efflux pumps enhances its survival in hostile environments, making it a formidable cause of nosocomial UTIs.
Key Contributing Factors:
- Prolonged catheterization
- Urological instrumentation or surgery
- Neurogenic bladder or obstruction
- Diabetes mellitus
- Long-term antibiotic exposure
- Hospital or ICU admission
Clinical Presentation of Serratia Complicated UTIs
Symptoms may be subtle or masked, especially in chronically ill or catheterized individuals. However, signs of upper urinary tract involvement or systemic infection often indicate a complicated course.
Common Clinical Features:
- Dysuria, urgency, or frequency (may be absent in catheterized patients)
- Foul-smelling or cloudy urine
- Lower abdominal or flank pain
- Fever and chills
- Hematuria
- Delirium or confusion in elderly patients
- Sepsis or shock in advanced cases
Diagnostic Evaluation for Serratia-Associated UTI
Timely identification of the pathogen and its resistance profile is essential in guiding effective therapy.
Diagnostic Workup:
- Urine culture and sensitivity: Confirm Serratia marcescens and assess antibiotic susceptibility.
- Urinalysis: Detects pyuria, nitrites, leukocyte esterase, and hematuria.
- Blood cultures: In febrile or septic patients to rule out bacteremia.
- Ultrasound or CT scan: To evaluate for urinary obstruction, abscess, or anatomical anomalies.
Antibiotic Resistance Patterns in Serratia UTIs
Serratia species exhibit intrinsic resistance to several commonly used antibiotics, including ampicillin, first-generation cephalosporins, and macrolides. The presence of inducible AmpC β-lactamases further complicates treatment.
Common Resistance Mechanisms:
- AmpC β-lactamase production
- Efflux pumps
- Porin loss
- Biofilm-related resistance
Frequently Ineffective Agents:
- Ampicillin
- Cephalexin
- Nitrofurantoin
- Fosfomycin
Evidence-Based Treatment of Serratia Complicated UTIs
Antibiotic therapy must be guided by susceptibility testing due to variable resistance profiles.
First-Line Options (based on sensitivities):
- Carbapenems (e.g., meropenem, ertapenem) for multidrug-resistant isolates
- Fluoroquinolones (e.g., ciprofloxacin, levofloxacin) in susceptible strains
- Third- or fourth-generation cephalosporins (e.g., cefepime, ceftazidime)
- Aminoglycosides (e.g., amikacin) as adjunctive therapy
Duration of Therapy:
- Uncomplicated Serratia UTI: 7–10 days
- Complicated cases with structural anomalies or bacteremia: 10–21 days
- Catheter-associated UTI: Remove or replace catheter and treat for at least 10 days
Management Strategies Beyond Antibiotics
Antimicrobial treatment alone may be insufficient without addressing the underlying causes or risk factors contributing to Serratia persistence.
Supportive and Interventional Measures:
- Prompt catheter removal or replacement
- Drainage of urinary tract obstruction
- Correction of anatomical defects
- Hydration to promote urinary flow
- Infectious disease consultation in resistant or recurrent cases
Prevention of Serratia-Related Urinary Infections
Due to the nosocomial nature of most Serratia UTIs, prevention hinges on meticulous infection control and judicious antibiotic use.
Proven Preventive Tactics:
- Aseptic catheter insertion techniques
- Minimize duration of catheterization
- Routine catheter care protocols
- Surveillance cultures in high-risk wards
- Antimicrobial stewardship programs
Complications of Untreated or Recurrent Serratia UTIs
Failure to effectively treat Serratia-related urinary infections may result in serious complications, particularly in vulnerable patient populations.
Potential Adverse Outcomes:
- Pyelonephritis
- Perinephric or renal abscess
- Urosepsis and septic shock
- Renal failure
- Chronic bacteriuria
- Hospital readmission and prolonged stays
Serratia UTIs in Immunocompromised Hosts
Individuals with weakened immunity, including transplant recipients, cancer patients, and the elderly, are highly susceptible to disseminated Serratia infections.
Clinical Considerations:
- Broader empiric coverage at initiation
- Vigilant monitoring for bacteremia
- Extended duration of therapy
- Multidisciplinary collaboration
Serratia complicated UTIs represent a growing clinical challenge due to their association with healthcare settings, resistance profiles, and potential for systemic complications. Accurate diagnosis, susceptibility-guided therapy, and aggressive management of risk factors are essential for optimal patient outcomes. Enhanced infection control and preventive strategies are paramount in reducing the burden of this opportunistic, drug-resistant pathogen.