Serratia bronchitis is a respiratory tract infection caused by the Serratia marcescens bacterium, a gram-negative, facultative anaerobe commonly associated with healthcare environments. Though typically an opportunistic pathogen, it can cause serious bronchial infections, particularly in immunocompromised patients, those with underlying lung disease, or individuals with indwelling respiratory devices. Given its potential resistance to multiple antibiotics, prompt recognition and treatment are crucial.
Pathogenesis and Risk Factors of Serratia Bronchitis
Serratia marcescens invades the lower respiratory tract, colonizing mucosal surfaces and producing enzymes that promote tissue damage and inflammation. The bacteria can form biofilms on endotracheal tubes, ventilators, or bronchoscopes, facilitating persistent infection and resistance to antibiotics.
Key Risk Factors:
- Hospitalization or ICU stay
- Mechanical ventilation
- Chronic obstructive pulmonary disease (COPD)
- Cystic fibrosis or bronchiectasis
- Prolonged antibiotic therapy
- Immunosuppression (e.g., chemotherapy, HIV)
Clinical Presentation of Serratia-Induced Bronchitis
The symptoms of Serratia bronchitis can resemble those of other bacterial or viral respiratory infections, but may persist longer and exhibit poor response to standard antibiotics.
Common Symptoms:
- Persistent productive cough with purulent sputum
- Shortness of breath or wheezing
- Fever, chills, or night sweats
- Chest discomfort
- Fatigue and malaise
- Hemoptysis in severe cases
In ventilated patients, changes in ventilator settings or declining oxygenation may be the only clues.
Diagnostic Evaluation for Serratia Bronchitis
Timely diagnosis is essential to prevent progression to pneumonia or sepsis. Diagnostic workup includes:
- Sputum culture and sensitivity: Confirms Serratia marcescens and identifies antimicrobial resistance.
- Bronchoalveolar lavage (BAL): Especially useful in intubated patients or when sputum samples are inadequate.
- Blood cultures: To rule out bacteremia.
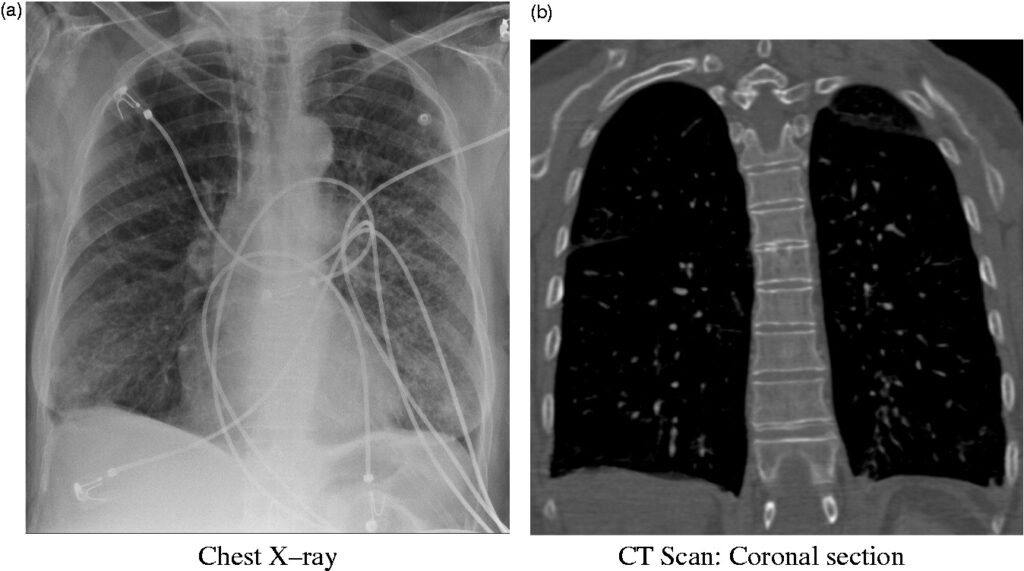
- Chest X-ray or CT scan: May show patchy infiltrates or bronchial wall thickening.
- Complete blood count (CBC) and inflammatory markers: Often show leukocytosis and elevated CRP.
Differentiation from other causes of chronic bronchitis (e.g., viral, fungal, or tuberculosis) is essential.
Antimicrobial Treatment of Serratia Bronchitis
Serratia marcescens often exhibits resistance to many first-line antibiotics, including penicillins and first-generation cephalosporins, due to production of inducible AmpC β-lactamases.
Empiric Therapy (Adjusted Based on Sensitivities):
- Carbapenems (e.g., meropenem, imipenem) for multidrug-resistant strains
- Fourth-generation cephalosporins (e.g., cefepime)
- Fluoroquinolones (e.g., ciprofloxacin) in mild cases
- Aminoglycosides (e.g., amikacin) may be added for synergy
Duration of Therapy:
- Uncomplicated cases: 10–14 days
- Complicated or immunocompromised patients: 14–21 days
Monitoring:
- Repeat cultures may be required in persistent or ventilator-associated cases.
- Renal and liver function tests during therapy.
Infection Control and Hospital Prevention
Serratia bronchitis is commonly associated with nosocomial transmission. Prevention depends heavily on strict infection control protocols.
Recommended Strategies:
- Sterile technique during intubation, suctioning, and bronchoscopy
- Regular decontamination of respiratory equipment
- Hand hygiene compliance
- Isolation precautions for infected patients
- Antibiotic stewardship to reduce emergence of resistant strains
Complications of Serratia Bronchitis
Without appropriate treatment, Serratia bronchitis can evolve into more severe pulmonary or systemic conditions.
Potential Complications:
- Serratia pneumonia
- Empyema or lung abscess
- Sepsis and septic shock
- Acute respiratory failure
- Colonization of other body sites (e.g., urinary tract, bloodstream)
Early intervention reduces the risk of these complications significantly.
Serratia Bronchitis in Immunocompromised Hosts
Patients with suppressed immunity, such as organ transplant recipients, cancer patients, or individuals with HIV/AIDS, are at elevated risk for recurrent or disseminated Serratia infections.
Tailored Considerations:
- Broader empiric antibiotic coverage pending cultures
- Longer treatment duration
- Closer clinical and radiologic follow-up
- Multidisciplinary management including infectious disease specialists
Serratia bronchitis represents a challenging, often underdiagnosed respiratory infection with significant potential for morbidity, particularly in healthcare settings. Accurate diagnosis, awareness of risk factors, and targeted antimicrobial therapy are essential for favorable outcomes. Adherence to infection control standards and antimicrobial stewardship are vital in preventing nosocomial spread and antibiotic resistance.