Serotonin syndrome is a potentially life-threatening condition resulting from excessive serotonergic activity in the central and peripheral nervous systems. It most commonly arises due to drug interactions, overdose, or therapeutic use of medications that enhance serotonin transmission. Rapid recognition and management are essential to prevent serious complications and mortality.
Pathophysiology of Serotonin Toxicity
Serotonin syndrome results from overstimulation of 5-HT1A and 5-HT2A receptors in the brain and spinal cord. Excessive serotonin activity disrupts autonomic, cognitive, and neuromuscular balance, producing a spectrum of clinical signs ranging from mild agitation to hyperthermia and seizures.
Medications and Substances Associated with Serotonin Syndrome
Several drug classes and combinations can precipitate serotonin syndrome. The most common culprits include:
Selective Serotonin Reuptake Inhibitors (SSRIs)
- Fluoxetine, sertraline, citalopram, paroxetine
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Venlafaxine, duloxetine
Monoamine Oxidase Inhibitors (MAOIs)
- Phenelzine, isocarboxazid, selegiline
Tricyclic Antidepressants (TCAs)
- Amitriptyline, clomipramine
Atypical Antidepressants and Others
- Trazodone, mirtazapine, lithium, buspirone
Illicit Substances and OTC Agents
- MDMA (ecstasy), LSD, dextromethorphan, St. John’s wort
High-risk combinations:
- SSRI + MAOI
- SNRI + triptan
- Linezolid + antidepressants
Clinical Features of Serotonin Syndrome
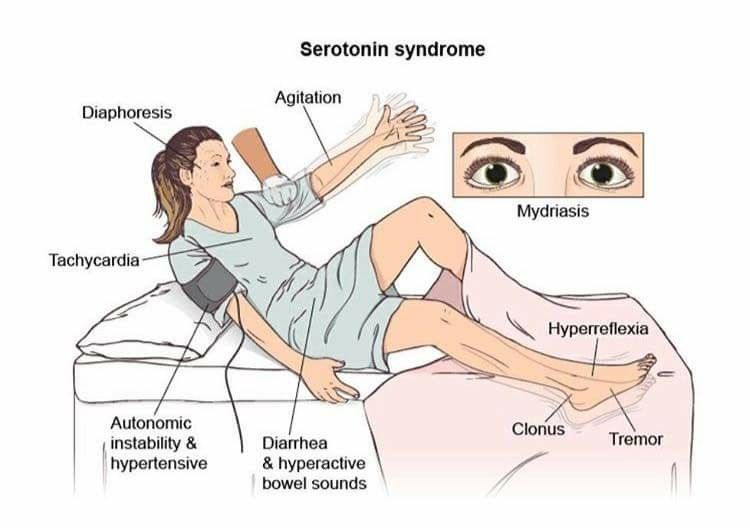
Symptoms typically develop within hours of initiating or increasing the serotonergic agent. The clinical presentation is characterized by the classic triad:
1. Neuromuscular Hyperactivity
- Hyperreflexia, myoclonus, tremor, bilateral clonus
- Muscle rigidity, especially in the lower limbs
2. Autonomic Instability
- Hyperthermia, tachycardia, hypertension
- Flushed skin, diaphoresis, shivering
3. Mental Status Changes
- Agitation, restlessness, anxiety
- Confusion, delirium, seizures in severe cases
In severe cases, symptoms may progress to rhabdomyolysis, metabolic acidosis, renal failure, or death.
Diagnostic Evaluation
Diagnosis is primarily clinical, with no definitive laboratory test. The Hunter Serotonin Toxicity Criteria is the most sensitive and specific tool for diagnosis in patients exposed to a serotonergic agent.
Hunter Criteria Includes:
- Spontaneous clonus
- Inducible clonus plus agitation or diaphoresis
- Ocular clonus plus agitation or diaphoresis
- Tremor plus hyperreflexia
- Hypertonia plus temperature >38°C and ocular or inducible clonus
Laboratory tests aid in ruling out differential diagnoses and assessing severity:
- CBC, electrolytes, renal and liver function
- CK levels to monitor rhabdomyolysis
- ABG for acid-base status
Differential diagnoses include neuroleptic malignant syndrome (NMS), anticholinergic toxicity, malignant hyperthermia, and meningitis.
Treatment of Serotonin Syndrome
Immediate Management
- Discontinue all serotonergic agents immediately
- Supportive care is the cornerstone of treatment
- Oxygen supplementation
- IV fluids for volume resuscitation
- External cooling for hyperthermia
Sedation and Symptom Control
- Benzodiazepines (e.g., lorazepam) to control agitation, tremor, and seizures
- Cyproheptadine, a serotonin antagonist, is useful in moderate to severe cases
- Initial dose: 12 mg orally, followed by 2 mg every 2 hours as needed
Advanced Interventions
- Intubation and paralysis for patients with extreme hyperthermia (>41.1°C)
- Avoid antipyretics, which are ineffective in serotonin syndrome
- Avoid physical restraints, which may worsen hyperthermia and lactic acidosis
Prognosis and Recovery
Most patients recover within 24 to 72 hours of discontinuing the offending agent and initiating treatment. Severe cases may require prolonged ICU care. Early recognition and prompt therapy dramatically improve prognosis.
Mortality is rare but can occur in severe, untreated cases involving profound hyperthermia, seizures, or multiorgan failure.
Prevention Strategies for Serotonin Syndrome
- Thorough medication reconciliation before initiating new serotonergic drugs
- Avoid combinations of high-risk serotonergic agents
- Educate patients on drug interaction risks and early symptom recognition
- Titrate serotonergic drugs slowly, especially in polypharmacy cases
- Use alternatives where possible in patients with prior serotonin syndrome
Serotonin syndrome remains an under-recognized but preventable medical emergency. Understanding its pathophysiology, identifying high-risk drug combinations, and initiating timely treatment are essential components of clinical practice. As the use of serotonergic medications continues to rise, vigilance among clinicians is critical to safeguarding patient safety.