Carcinoma in situ (CIS) of the glans penis, also referred to as erythroplasia of Queyrat, is a rare but serious premalignant condition. It represents the early stages of penile cancer, where abnormal cells are confined to the epithelial layer of the glans. Early detection and treatment are crucial to prevent progression to invasive carcinoma. This article explores the causes, clinical presentation, diagnostic methods, and treatment strategies for this condition.
Pathophysiology and Risk Factors
What Is Carcinoma In Situ of the Glans Penis?
CIS of the glans penis is a form of squamous cell carcinoma limited to the epithelial surface. Unlike invasive cancer, CIS has not penetrated deeper layers of tissue or metastasized.
Risk Factors
Several factors increase the likelihood of developing carcinoma in situ of the glans penis:
- Human Papillomavirus (HPV) Infection: High-risk HPV strains, such as HPV-16 and HPV-18, are strongly associated with CIS.
- Phimosis: Chronic inability to retract the foreskin increases susceptibility to irritation and infections.
- Poor Hygiene: Accumulation of smegma may contribute to chronic inflammation.
- Immunosuppression: Conditions such as HIV or post-organ transplantation immunosuppression elevate the risk.
- Tobacco Use: Smoking has been linked to an increased risk of squamous cell carcinoma, including CIS.
Clinical Features
Symptoms
Patients with carcinoma in situ of the glans penis often present with:
- Persistent reddish patches or lesions on the glans
- Itching, burning, or discomfort in the affected area
- Ulceration or erosion that does not heal
- Thickened or raised areas of skin
Differential Diagnosis
Other conditions that may mimic CIS include:
- Psoriasis
- Lichen planus
- Balanitis
- Paget’s disease
- Bowenoid papulosis
Diagnostic Approach
Physical Examination
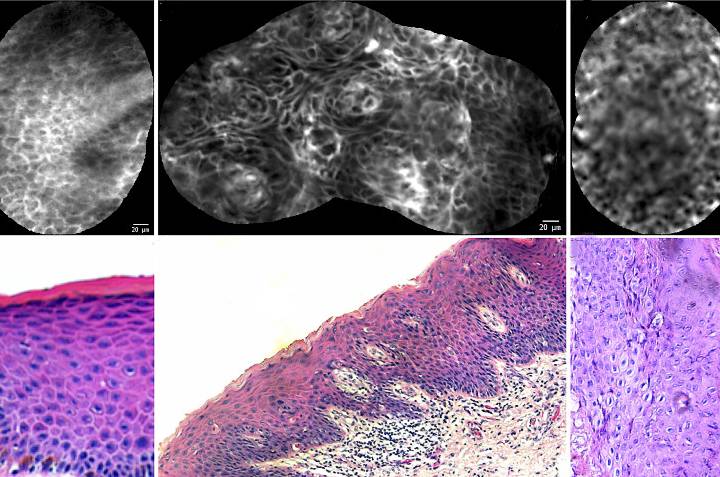
A thorough clinical examination is essential. The lesions are typically well-demarcated, erythematous, and may appear velvety or ulcerative.
Biopsy
A definitive diagnosis is achieved through a biopsy, either incisional or excisional, followed by histopathological analysis.
Imaging
Imaging studies, such as MRI or ultrasound, are used to assess the extent of the lesion and exclude invasive cancer.
Treatment Modalities
Topical Therapies
- 5-Fluorouracil (5-FU): An effective chemotherapeutic agent applied locally.
- Imiquimod: A topical immune response modifier that enhances the immune system’s ability to target abnormal cells.
Surgical Options
- Laser Ablation: CO2 or Nd:YAG lasers are often used for precise removal of the lesion.
- Mohs Micrographic Surgery: Provides high cure rates by ensuring complete removal of cancerous cells while sparing healthy tissue.
Photodynamic Therapy (PDT)
PDT involves the application of photosensitizing agents followed by light activation, selectively destroying cancerous cells.
Penile-Sparing Techniques
Whenever feasible, penile-sparing techniques are prioritized to maintain function and appearance.
Total or Partial Penectomy
In cases where invasive cancer is suspected or confirmed, surgical removal of part or all of the penis may be necessary.
Prognosis
With early diagnosis and appropriate treatment, the prognosis for carcinoma in situ of the glans penis is excellent. However, untreated cases can progress to invasive cancer, significantly worsening outcomes.
Prevention
- HPV Vaccination: Vaccines like Gardasil can reduce the risk of high-risk HPV strains.
- Safe Sexual Practices: Using condoms reduces HPV transmission.
- Good Genital Hygiene: Regular cleaning of the genital area helps prevent irritation and infections.
- Routine Medical Check-Ups: Early detection through regular examinations is crucial.