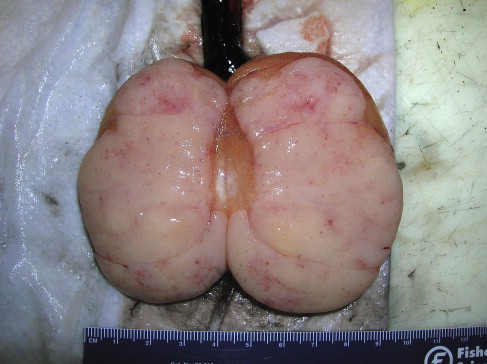
Seminoma of the testis is a malignant germ cell tumor, accounting for approximately 50% of all testicular cancers. It typically affects males between the ages of 25 and 45 and arises from the germinal epithelium of the seminiferous tubules. Due to its high sensitivity to radiation and chemotherapy, seminoma generally carries a favorable prognosis when detected early.
Epidemiology and Risk Factors
Incidence and Demographics
Seminoma represents the most common subtype of testicular germ cell tumors in Western populations. Incidence rates have been increasing, with the highest frequency observed in Caucasian males.
Recognized Risk Factors
- Cryptorchidism (undescended testis)
- Family history of testicular cancer
- Klinefelter syndrome (for non-seminomatous GCTs)
- Infertility and testicular dysgenesis syndrome
- Previous history of testicular cancer in the contralateral testis
Pathophysiology and Histological Features
Seminoma originates from primordial germ cells, typically confined within the testis at the time of diagnosis. Histologically, seminomas are characterized by:
- Sheets of uniform polygonal cells with clear cytoplasm
- Prominent central nucleoli
- Abundant lymphocytic infiltrate in the stroma
- Absence of serum alpha-fetoprotein (AFP) elevation (a key distinguishing feature)
Clinical Presentation and Diagnostic Evaluation
Symptoms and Physical Findings
Patients commonly present with:
- Painless testicular mass (most frequent sign)
- Scrotal heaviness or discomfort
- Rarely, symptoms from metastatic spread (e.g., back pain due to retroperitoneal lymphadenopathy)
Diagnostic Workup
- Scrotal Ultrasound: Reveals a hypoechoic, homogeneous intratesticular lesion.
- Tumor Markers:
- Beta-hCG: May be elevated in ~15–20% of seminomas
- AFP: Not elevated (differentiates seminoma from non-seminomatous tumors)
- LDH: May correlate with tumor burden
- Cross-sectional Imaging:
- CT scan of chest, abdomen, and pelvis for staging and lymph node involvement
- Radical Inguinal Orchiectomy: Diagnostic and therapeutic; trans-scrotal biopsy is contraindicated due to risk of tumor seeding.
Treatment of Seminoma by Stage
Stage I Seminoma
- Radical Inguinal Orchiectomy is the primary intervention.
- Post-Orchiectomy Options:
- Active Surveillance: Preferred for low-risk patients (relapse rate ~15–20%)
- Adjuvant Radiotherapy: Historically used, now declining due to long-term risks
- Single-agent Carboplatin Chemotherapy: Comparable relapse prevention
Stage II Seminoma
- Stage IIA/B (small-volume retroperitoneal disease):
- Radiotherapy to para-aortic and pelvic nodes
- Cisplatin-based chemotherapy for higher nodal burden
- Stage IIC (bulky disease):
- Primary chemotherapy (BEP regimen: Bleomycin, Etoposide, Cisplatin)
Stage III Seminoma
- Advanced or metastatic disease
- Systemic Chemotherapy: 3–4 cycles of BEP or EP (Etoposide + Cisplatin)
- Post-chemotherapy Residual Mass:
- PET scan if mass >3 cm
- Surgical resection if viable tumor suspected
Prognosis and Survival Rates
Prognostic Classification (IGCCCG Criteria)
- Good Prognosis:
- No non-pulmonary visceral metastases
- Normal or mildly elevated markers
- 5-year survival: >90%
- Intermediate Prognosis:
- Non-pulmonary visceral metastases
- 5-year survival: ~75–80%
Surveillance After Treatment
- Regular clinical exams
- Serial imaging (CT chest/abdomen/pelvis)
- Tumor marker assessment (Beta-hCG, LDH)
Typical schedule: Every 3–6 months for first 2 years, then annually.
Long-Term Considerations and Fertility Preservation
Secondary Malignancy and Cardiovascular Risk
- Risk increases with radiotherapy and chemotherapy exposure
- Lifestyle modifications and routine follow-up are essential
Fertility Management
- Sperm banking before treatment is strongly advised
- Testosterone levels may need monitoring post-orchiectomy
Future Perspectives and Research Directions
- Molecular profiling for personalized therapy
- Minimally invasive management of residual masses
- Immunotherapy exploration for refractory disease
Seminoma of the testis is a curable malignancy with excellent prognosis when treated appropriately. Timely diagnosis, accurate staging, and personalized treatment strategies remain the cornerstone of effective management. Advances in imaging, chemotherapy regimens, and surveillance protocols continue to enhance long-term outcomes for affected individuals.