Tuberous sclerosis complex (TSC) is a rare autosomal dominant genetic disorder characterized by the growth of benign tumors in multiple organ systems, including the brain. The central nervous system involvement, particularly cortical tubers, subependymal nodules, and subependymal giant cell astrocytomas (SEGAs), plays a pivotal role in the pathogenesis of epilepsy in TSC patients.
Epilepsy is the most common neurological manifestation of TSC, affecting approximately 80–90% of individuals with the condition. Seizures often begin in infancy and are frequently refractory to conventional treatments, leading to significant cognitive and developmental impairment.
Pathophysiology of Seizures in Tuberous Sclerosis Complex
Molecular and Cellular Mechanisms
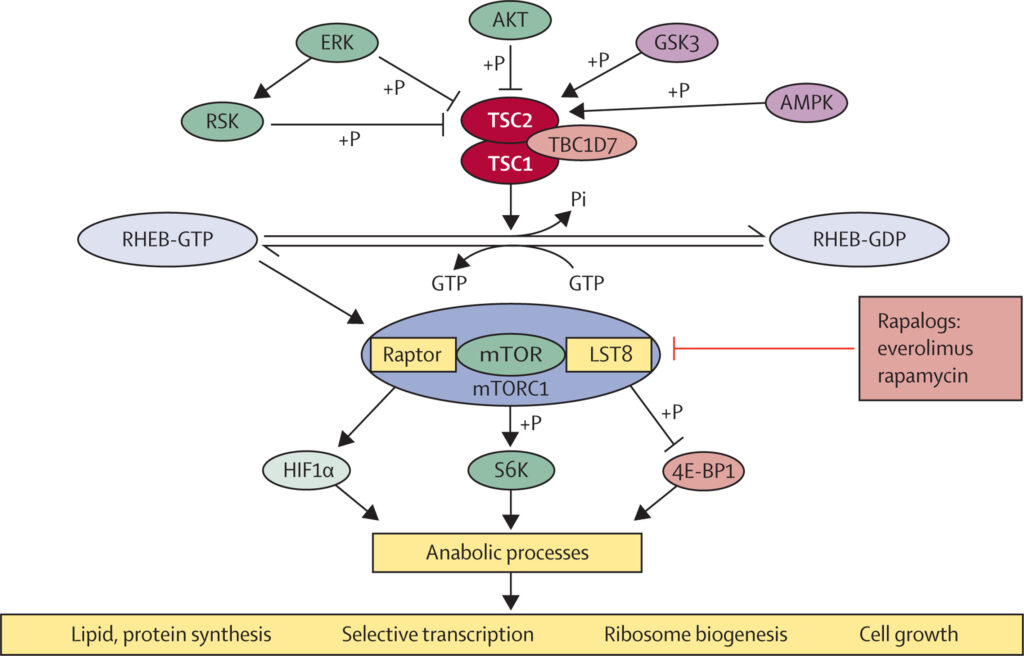
TSC results from mutations in either the TSC1 or TSC2 genes, which encode hamartin and tuberin, respectively. These proteins inhibit the mammalian target of rapamycin (mTOR) pathway, a key regulator of cell growth and proliferation.
When this pathway is dysregulated:
- Abnormal neural development occurs
- Cortical tubers form, disrupting normal neuronal circuitry
- Epileptogenic zones are created in structurally abnormal areas
Clinical Spectrum of Seizures in TSC
Seizure Types and Onset
Seizures typically present within the first year of life, often as:
- Infantile spasms (West syndrome)
- Focal seizures with or without impaired awareness
- Tonic or atonic seizures
- Generalized tonic-clonic seizures
Early onset, particularly before the age of 1, is associated with worse developmental outcomes.
EEG Findings
Electroencephalographic patterns vary widely but commonly demonstrate:
- Multifocal epileptiform discharges
- Hypsarrhythmia in infantile spasms
- Background slowing
- Ictal onset corresponding to cortical tubers
Diagnostic Evaluation of TSC-Associated Epilepsy
Neuroimaging
MRI of the brain reveals:
- Cortical tubers (hyperintense on T2-weighted and FLAIR sequences)
- Subependymal nodules
- SEGAs near the foramen of Monro
These abnormalities are typically bilateral and widespread.
Genetic Testing
Molecular testing confirms mutations in TSC1 or TSC2 genes, aiding in diagnosis and familial counseling. Genotype-phenotype correlations suggest TSC2 mutations are linked to earlier and more severe epilepsy.
Therapeutic Management of Seizures in Tuberous Sclerosis Complex
Pharmacologic Treatments
Effective seizure control in TSC requires targeted and aggressive therapy:
- Vigabatrin: First-line for infantile spasms in TSC; acts as a GABA transaminase inhibitor
- Everolimus: An mTOR inhibitor approved for TSC-associated seizures, reducing seizure frequency by modulating the underlying molecular pathway
- Levetiracetam, topiramate, clobazam: Frequently used adjunctive therapies
Non-Pharmacologic Approaches
- Ketogenic diet: Particularly effective in drug-resistant epilepsy
- Vagus nerve stimulation (VNS): Beneficial in select refractory cases
- Surgical resection: Targeted resection of epileptogenic tubers offers the best chance of long-term seizure freedom
Role of Epilepsy Surgery in TSC
Candidate Selection and Pre-Surgical Workup
Surgical intervention is considered when seizures are focal and originate from discrete cortical tubers. Evaluation includes:
- Video EEG monitoring
- Magnetoencephalography (MEG)
- Functional MRI
- PET or SPECT imaging
Outcomes
- Seizure-free rates range from 50–70% in selected candidates
- Surgery is most effective when performed early in life, ideally before cognitive decline becomes irreversible
Developmental and Cognitive Implications of Seizures in TSC
Persistent and uncontrolled seizures are a major contributor to TSC-associated neuropsychiatric disorders (TAND), which include:
- Intellectual disability
- Autism spectrum disorder
- Behavioral disturbances
Early seizure control correlates strongly with improved developmental outcomes, reinforcing the need for proactive management.
Emerging and Investigational Therapies
New mTOR Pathway Inhibitors
Ongoing studies are assessing newer mTOR inhibitors with improved safety profiles and enhanced brain penetration to treat epilepsy more effectively.
Gene-Targeted Approaches
Though still experimental, gene therapy and antisense oligonucleotides (ASOs) targeting TSC mutations represent future therapeutic strategies with the potential to modify disease progression.
Long-Term Management and Prognosis
Multidisciplinary Care
Successful management requires collaboration among:
- Pediatric neurologists
- Epileptologists
- Neurosurgeons
- Developmental specialists
- Genetic counselors
Monitoring and Follow-Up
- Regular EEGs and brain MRIs
- Seizure diaries and developmental assessments
- Everolimus blood level monitoring when applicable
Seizures in tuberous sclerosis complex are a defining and often debilitating feature of the disease, particularly in early life. Due to their high prevalence and resistance to conventional treatments, a tailored approach involving early diagnosis, mTOR-targeted therapies, and surgical consideration is imperative. Ongoing advances in molecular and gene-based therapies hold promise for transforming long-term outcomes in individuals with TSC-related epilepsy.

