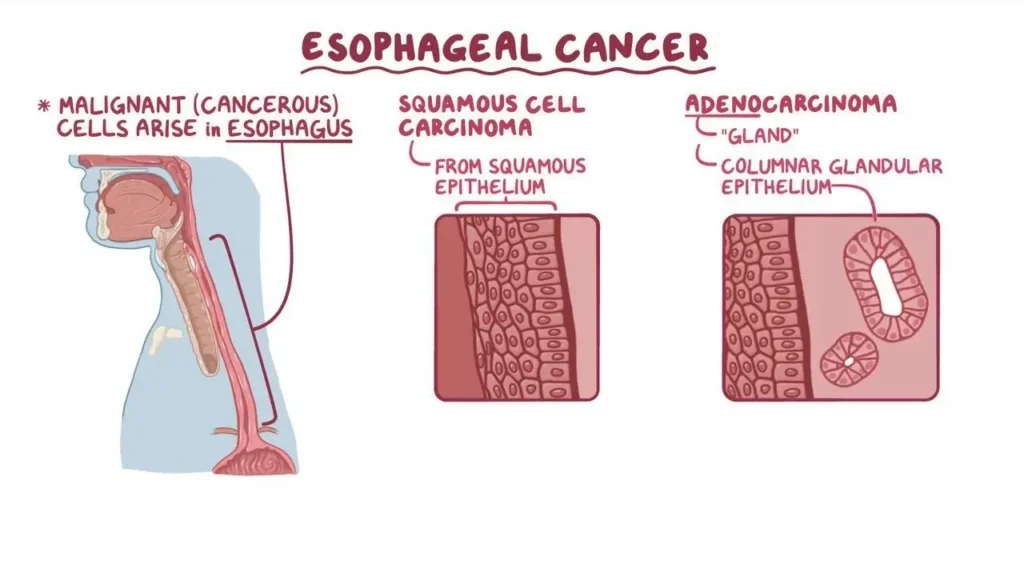
Carcinoma in situ (CIS) of the esophagus is a precancerous condition that represents the earliest form of esophageal cancer. At this stage, abnormal cells are present only in the innermost lining of the esophagus and have not invaded deeper tissues. Early detection and timely intervention are critical in preventing progression to invasive cancer.
Understanding Carcinoma in Situ of the Esophagus
Definition and Pathophysiology
Carcinoma in situ of the esophagus involves the presence of dysplastic, abnormal cells confined to the epithelial layer. This condition is often associated with chronic irritation or damage to the esophageal lining due to factors such as gastroesophageal reflux disease (GERD) or Barrett’s esophagus. Over time, genetic mutations in these cells may lead to unregulated growth, marking the transition to cancer if untreated.
Causes and Risk Factors
Several factors contribute to the development of esophageal CIS:
- Chronic GERD: Prolonged acid exposure can damage the esophageal lining, increasing the risk of cellular changes.
- Barrett’s Esophagus: A condition in which the normal squamous epithelium is replaced by columnar epithelium, predisposing individuals to dysplasia.
- Tobacco and Alcohol Use: Both substances can irritate the esophagus and contribute to carcinogenesis.
- Obesity: Linked to increased GERD prevalence and esophageal irritation.
- Dietary Factors: Low intake of fruits and vegetables and high consumption of processed or hot beverages may elevate risk.
Clinical Presentation
Symptoms
Carcinoma in situ is often asymptomatic, particularly in its early stages. However, symptoms may include:
- Persistent heartburn or acid reflux
- Difficulty swallowing (dysphagia)
- Unexplained weight loss
- Chest discomfort
Diagnosis
Accurate diagnosis requires a combination of the following approaches:
- Endoscopy: Visual inspection of the esophageal lining to detect abnormalities.
- Biopsy: Collection of tissue samples for histological examination.
- Imaging: Advanced techniques like endoscopic ultrasound (EUS) can assess the extent of cellular changes.
Biopsy Findings
Biopsy results typically reveal:
- Dysplastic cells confined to the mucosal layer
- No invasion into the submucosa or beyond
Treatment Options
Endoscopic Interventions
Minimally invasive procedures are often the first line of treatment for esophageal CIS:
- Endoscopic Mucosal Resection (EMR): Removal of the affected mucosal layer using endoscopic tools.
- Radiofrequency Ablation (RFA): Application of heat energy to destroy dysplastic cells.
- Cryotherapy: Freezing and eliminating abnormal tissue using liquid nitrogen or carbon dioxide.
Surgical Treatment
In rare cases, where CIS is extensive or unresponsive to endoscopic therapies, esophagectomy (removal of part or all of the esophagus) may be recommended.
Pharmacological Management
- Proton Pump Inhibitors (PPIs): Reduce acid reflux, minimizing further esophageal damage.
- Aspirin or NSAIDs: Investigated for their role in chemoprevention.
Prognosis and Monitoring
Prognosis
When treated promptly, the prognosis for carcinoma in situ is excellent, with high survival rates and a low likelihood of progression to invasive cancer.
Follow-Up Care
Regular monitoring is essential to detect recurrence or progression:
- Scheduled Endoscopies: Typically every 3-6 months initially, then annually.
- Biopsy: Periodic sampling to ensure no residual dysplasia.
Prevention Strategies
- Lifestyle Modifications:
- Avoid tobacco and limit alcohol consumption.
- Maintain a healthy weight.
- Incorporate a diet rich in fruits, vegetables, and whole grains.
- Management of GERD:
- Use of PPIs and lifestyle changes to control acid reflux.
- Screening Programs:
- Routine endoscopies for individuals with Barrett’s esophagus or high-risk factors.