Isoniazid (INH) is a frontline antitubercular medication, but in overdose situations, it poses a serious neurotoxic threat, most notably by inducing seizures. These seizures are often refractory to conventional antiepileptic drugs and require specific antidotal therapy. Understanding the pathophysiology, clinical manifestations, and evidence-based interventions is crucial in managing INH toxicity effectively.
Pathophysiology of Seizures in Isoniazid Overdose
Mechanism of Neurotoxicity
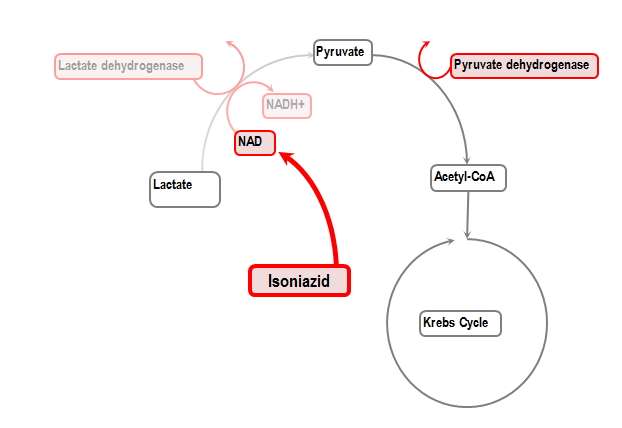
Isoniazid interferes with gamma-aminobutyric acid (GABA) synthesis by depleting pyridoxine (vitamin B6), an essential cofactor in the enzymatic production of GABA from glutamate. This disruption lowers the inhibitory tone in the central nervous system, leading to neuronal hyperexcitability and seizures.
Clinical Features of Isoniazid Toxicity
Symptom Onset and Progression
Symptoms typically appear within 30 minutes to 2 hours post-ingestion, especially in acute overdose scenarios. Clinical features include:
- Neurologic Symptoms:
- Refractory generalized tonic-clonic seizures
- Agitation and altered mental status
- Coma in severe cases
- Metabolic Disturbances:
- Lactic acidosis
- Hypoglycemia (occasionally)
- Cardiovascular Effects:
- Tachycardia
- Hypotension (with massive overdose)
Diagnostic Approach in Suspected INH-Induced Seizures
Clinical Diagnosis
Diagnosis is primarily clinical, particularly when there is a known history of INH ingestion. High suspicion is warranted in the following contexts:
- Known tuberculosis treatment or suicide attempt
- Sudden onset of seizures unresponsive to benzodiazepines
- Anion gap metabolic acidosis
Laboratory Workup
- Arterial blood gas: Metabolic acidosis
- Serum lactate: Elevated due to seizures and tissue hypoxia
- Liver enzymes: May be mildly elevated
- Glucose, electrolytes, renal function: Rule out contributing factors
- Blood INH level (not readily available in emergencies)
Emergency Management of INH Toxicity and Seizures
Immediate Interventions
- Airway, Breathing, Circulation (ABCs): Stabilize vitals and secure airway if altered mental status or recurrent seizures occur.
- Seizure Control:
- Initial step: Benzodiazepines (e.g., lorazepam) IV
- Essential therapy: Pyridoxine (Vitamin B6) – this directly reverses INH-induced GABA depletion
Pyridoxine Administration Protocol
- Dose: 1 gram IV for every gram of INH ingested, or 70 mg/kg IV if ingestion amount is unknown
- Administration: Given over 30 minutes, may be repeated if seizures persist
Adjunctive Therapies
- Intravenous fluids for hemodynamic support
- Sodium bicarbonate for severe metabolic acidosis
- Mechanical ventilation if respiratory failure develops
- Hemodialysis: Considered in massive overdoses, renal failure, or persistent metabolic derangements
Special Considerations in Pediatric and Chronic INH Use
Pediatric Ingestion
Children are particularly vulnerable to INH toxicity, even at relatively low doses. A single adult tablet may induce seizures in a small child. Prompt administration of pyridoxine is critical to avoid irreversible neurologic damage.
Chronic Use and Subclinical Neurotoxicity
Patients on long-term isoniazid therapy may experience peripheral neuropathy due to gradual pyridoxine depletion. This is prevented by co-administering prophylactic pyridoxine (10–50 mg/day), especially in individuals with malnutrition, HIV, diabetes, or renal insufficiency.
Prognosis and Outcomes
With timely diagnosis and administration of pyridoxine, most patients recover fully from INH-induced seizures. However, delays in treatment or inadequate pyridoxine dosing can result in prolonged seizures, hypoxic brain injury, or death.
Prognostic indicators:
- Rapid reversal of seizures post-pyridoxine = favorable outcome
- Persistent coma or multi-organ dysfunction = poor prognosis
Prevention and Education
Safe Prescribing and Storage
- Educate patients on proper storage of INH, especially in households with children
- Limit quantities dispensed to reduce overdose risk
- Co-prescription of pyridoxine in high-risk populations
Awareness Among Clinicians
- Include INH toxicity in differential for unexplained seizures
- Maintain a high index of suspicion in patients with TB treatment history
- Stock pyridoxine in emergency and ICU settings as a critical antidote
Isoniazid toxicity is a life-threatening condition characterized by rapid-onset seizures that are unresponsive to standard anticonvulsants. These seizures are a direct result of pyridoxine depletion and consequent GABA synthesis impairment. The cornerstone of management is immediate pyridoxine administration, which rapidly reverses the pathophysiological effects and stabilizes the patient. Early recognition, clinical suspicion, and prompt therapy are key to preventing morbidity and mortality in INH-induced seizures.