Sedation refers to the administration of pharmacologic agents to reduce anxiety, discomfort, and awareness during medical or dental procedures. Its use spans a broad spectrum, from minimal sedation where patients remain responsive, to deep sedation and general anesthesia requiring airway support. Sedation enhances procedural success and patient cooperation while prioritizing safety and comfort.

Levels of Sedation and Their Clinical Indications
Understanding the continuum of sedation depth is crucial for appropriate clinical application and monitoring.
Minimal Sedation (Anxiolysis)
- Effect: Relieves anxiety with minimal cognitive impairment.
- Patient Response: Fully responsive to verbal commands.
- Common Use: Pre-diagnostic imaging, minor dental procedures.
Moderate Sedation (Conscious Sedation)
- Effect: Depresses consciousness without loss of protective reflexes.
- Patient Response: Purposeful response to verbal or light tactile stimulation.
- Common Use: Endoscopy, minor surgical procedures, interventional radiology.
Deep Sedation
- Effect: Patient not easily arousable but responds to repeated or painful stimulation.
- Patient Response: Potential for airway compromise, requiring vigilant monitoring.
- Common Use: Cardioversion, pediatric imaging, painful orthopedic reductions.
General Anesthesia
- Effect: Complete unconsciousness with loss of protective reflexes.
- Patient Response: No response to stimuli, requires airway and cardiovascular support.
- Common Use: Major surgeries and procedures requiring complete immobility.
Common Sedative Agents and Their Pharmacology
Benzodiazepines
- Examples: Midazolam, Diazepam
- Action: Enhance GABA activity; produce anxiolysis, amnesia
- Use: Moderate sedation, premedication
Opioids
- Examples: Fentanyl, Morphine
- Action: μ-opioid receptor agonists; analgesia and sedation
- Use: Combined with benzodiazepines for procedural sedation
Propofol
- Action: GABA-agonist; rapid onset and offset
- Use: Deep sedation and general anesthesia
- Note: Requires airway management skills due to respiratory depression
Ketamine
- Action: NMDA receptor antagonist; dissociative anesthesia
- Use: Pediatric sedation, patients with asthma, hypotension
- Advantages: Preserves airway reflexes and cardiovascular stability
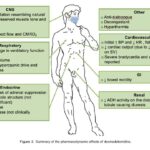
Dexmedetomidine
- Action: α2-adrenergic agonist; provides sedation without respiratory depression
- Use: ICU sedation, awake fiberoptic intubation
Procedural Sedation Protocol and Monitoring Standards
Pre-Sedation Evaluation
- Medical History Review: ASA classification, allergies, prior sedation reactions
- Airway Assessment: Mallampati score, neck mobility, obesity
- Informed Consent: Risks, benefits, alternatives discussed
Intra-Procedure Monitoring
| Parameter | Monitoring Tool | Frequency |
|---|---|---|
| Oxygen saturation | Pulse oximetry | Continuous |
| Heart rate and rhythm | ECG | Continuous |
| Blood pressure | Non-invasive cuff | Every 5 minutes |
| Respiratory rate | Clinical observation or capnography | Continuous |
Emergency Preparedness
- Immediate access to:
- Suction
- Bag-valve-mask ventilation
- Airway adjuncts
- Reversal agents (e.g., flumazenil, naloxone)
- Defibrillator and crash cart
Sedation Reversal Agents
| Drug | Indicated for Reversal of | Dose |
|---|---|---|
| Flumazenil | Benzodiazepines | 0.2 mg IV |
| Naloxone | Opioids | 0.1–0.2 mg IV |
Risks and Complications of Sedation
While sedation is generally safe under skilled administration, potential complications include:
- Respiratory depression
- Hypotension or bradycardia
- Airway obstruction
- Aspiration
- Allergic reactions or paradoxical excitation
Proper screening, dosing, and real-time monitoring significantly mitigate these risks.
Sedation in Special Populations
Pediatric Patients
- Require age-appropriate sedation protocols.
- Non-pharmacologic methods (distraction, parental presence) may enhance efficacy.
- Agents like ketamine and midazolam are preferred for safety and efficacy.
Geriatric Patients
- Increased sensitivity to sedatives.
- Risk of prolonged recovery, delirium, respiratory complications.
- Dose titration and slow administration essential.
Patients with Comorbidities
- Renal or hepatic impairment affects drug clearance.
- Obesity and OSA increase risk of airway compromise.
- Tailored approach needed with multidisciplinary support.
Legal and Ethical Considerations
- Credentialing: Only trained personnel should administer moderate or deep sedation.
- Documentation: Baseline vitals, consent, drug dosing, and recovery parameters must be recorded.
- Post-procedure Care: Clear discharge criteria, recovery scoring (e.g., Aldrete), and escort requirements for outpatient cases.
Sedation is a fundamental component of modern medicine, enabling patient comfort, procedural success, and clinical efficiency. Its safe application requires a comprehensive understanding of pharmacology, patient assessment, monitoring, and emergency management. With standardized protocols and vigilant care, sedation can be safely delivered across diverse clinical settings.