Secondary amenorrhea is defined as the absence of menstrual periods for three or more consecutive cycles—or six months—in women who previously had regular menstruation. Unlike primary amenorrhea, which refers to the failure to begin menstruation by age 15, secondary amenorrhea arises after menarche has already occurred.
This condition is not a disease itself but a symptom of an underlying physiological, hormonal, or structural abnormality. Timely evaluation is essential to determine the root cause and implement appropriate management.
Primary Causes of Secondary Amenorrhea
The etiology of secondary amenorrhea is diverse and can be classified into four major categories: hypothalamic, pituitary, ovarian, and uterine. Additional contributing factors include stress, extreme weight loss, and certain medications.
1. Hypothalamic Dysfunction (Functional Hypothalamic Amenorrhea)
- Triggered by stress, excessive exercise, or significant caloric restriction
- Suppresses gonadotropin-releasing hormone (GnRH) secretion
- Leads to decreased luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
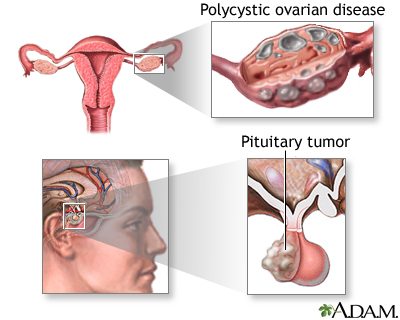
2. Pituitary Disorders
- Prolactinoma (pituitary adenoma) causing elevated prolactin, which suppresses gonadotropins
- Sheehan’s syndrome due to postpartum pituitary infarction
- Tumors or trauma affecting pituitary hormone output
3. Ovarian Causes
- Polycystic Ovary Syndrome (PCOS): most common cause; presents with hyperandrogenism, chronic anovulation, and polycystic ovaries
- Premature Ovarian Insufficiency (POI): cessation of ovarian function before age 40
- Surgical removal or damage due to chemotherapy or radiation
4. Uterine Causes
- Asherman’s syndrome: intrauterine adhesions usually from dilation and curettage (D&C)
- Congenital or acquired uterine abnormalities
Risk Factors Associated with Secondary Amenorrhea
- Intense athletic training
- Eating disorders such as anorexia nervosa or bulimia
- Chronic stress or psychiatric illness
- Thyroid disorders (both hyperthyroidism and hypothyroidism)
- Use of antipsychotics, antidepressants, contraceptives, or chemotherapy agents
Clinical Presentation and Symptoms
The hallmark of secondary amenorrhea is the cessation of menstruation. However, associated symptoms can provide clues about the underlying pathology.
| Symptom | Possible Cause |
|---|---|
| Galactorrhea (milk discharge) | Prolactinoma |
| Acne, hirsutism | PCOS, adrenal hyperplasia |
| Hot flashes, night sweats | Premature ovarian insufficiency |
| Weight loss, fatigue | Hypothalamic dysfunction |
| Visual disturbances | Pituitary tumor |
Diagnostic Evaluation of Secondary Amenorrhea
A stepwise and structured approach is required to identify the cause.
Key Investigations:
- β-hCG Test: Mandatory to exclude pregnancy
- FSH & LH Levels: Distinguish ovarian failure vs hypothalamic causes
- Prolactin: Elevated in prolactinoma
- TSH: Evaluate thyroid function
- Pelvic ultrasound: Assess uterine and ovarian anatomy
- MRI Brain: Indicated for suspected pituitary tumors
Hormonal Challenge Tests
Progesterone Challenge Test
- Administer medroxyprogesterone for 5–10 days
- Withdrawal bleeding indicates sufficient estrogen and an intact outflow tract
- No bleeding suggests low estrogen or anatomical obstruction
Estrogen-Progesterone Challenge
- Administer estrogen followed by progesterone
- Bleeding confirms a non-obstructed uterus and lack of endogenous estrogen
Treatment Approaches Based on Etiology
Functional Hypothalamic Amenorrhea
- Nutritional rehabilitation
- Reduced exercise intensity
- Stress management or cognitive behavioral therapy
Hyperprolactinemia
- Dopamine agonists such as cabergoline or bromocriptine
- Surgical resection for large or unresponsive prolactinomas
Polycystic Ovary Syndrome (PCOS)
- Lifestyle modifications: weight loss, low-glycemic diet
- Oral contraceptives to regulate cycles
- Metformin to improve insulin sensitivity
- Anti-androgens for hirsutism or acne
Premature Ovarian Insufficiency (POI)
- Hormone replacement therapy (HRT) to maintain bone and cardiovascular health
- Emotional support and fertility counseling
Asherman’s Syndrome
- Hysteroscopic lysis of adhesions
- Estrogen therapy to promote endometrial regeneration
Potential Complications of Untreated Secondary Amenorrhea
- Infertility due to chronic anovulation
- Osteopenia or osteoporosis from hypoestrogenism
- Cardiovascular risks associated with estrogen deficiency
- Psychosocial impact such as depression or anxiety
- Endometrial hyperplasia in unopposed estrogen states like PCOS
Fertility Considerations and Reproductive Options
Many causes of secondary amenorrhea are reversible with proper treatment, allowing restoration of ovulation and natural conception. For persistent ovarian failure, assisted reproductive technologies such as in vitro fertilization (IVF) with donor eggs may be necessary. Regular monitoring and early intervention improve outcomes significantly.
Preventive Measures and Long-Term Monitoring
- Maintain a healthy BMI (18.5–24.9)
- Moderate exercise without energy imbalance
- Avoid extreme dieting or fasting
- Regular gynecological evaluations
- Monitor bone density in long-term hypoestrogenic states
Secondary amenorrhea is a critical indicator of underlying hormonal or structural dysfunction. Accurate diagnosis and prompt, individualized treatment are essential to restore menstrual health and prevent long-term complications. With multidisciplinary care, most patients can achieve hormonal balance, preserve fertility, and maintain quality of life.