Seasonal Affective Disorder (SAD) is a recurring form of depression with a seasonal pattern, most commonly emerging during the fall and winter months. This condition is characterized by mood changes, lethargy, and diminished interest in daily activities. SAD poses a substantial burden on mental health, productivity, and quality of life. A strategic approach encompassing clinical diagnosis, light-based interventions, and preventive behavioral modifications is essential for effective long-term management.
Defining Seasonal Affective Disorder and Its Distinctive Pattern
Seasonal Affective Disorder is classified under major depressive disorder with seasonal pattern. Unlike typical depression, SAD is temporally linked to seasonal light variation. The most prevalent form, winter-pattern SAD, typically begins in late autumn and resolves in early spring.
Types of SAD
- Winter-pattern SAD: More common; onset in fall or winter
- Summer-pattern SAD: Rare; symptoms begin in spring or early summer
Etiology and Pathophysiology: The Role of Light and Neurobiology
The onset of SAD is closely associated with reduced daylight exposure and subsequent alterations in circadian rhythms and neurotransmitter function.
Pathophysiological Mechanisms
- Melatonin Dysregulation:
Increased melatonin production due to darkness leads to excessive sleepiness and fatigue. - Serotonin Deficiency:
Decreased sunlight may lower serotonin levels, contributing to depressive symptoms. - Circadian Rhythm Disruption:
Shortened daylight hours interfere with the body’s biological clock, leading to mood imbalances.
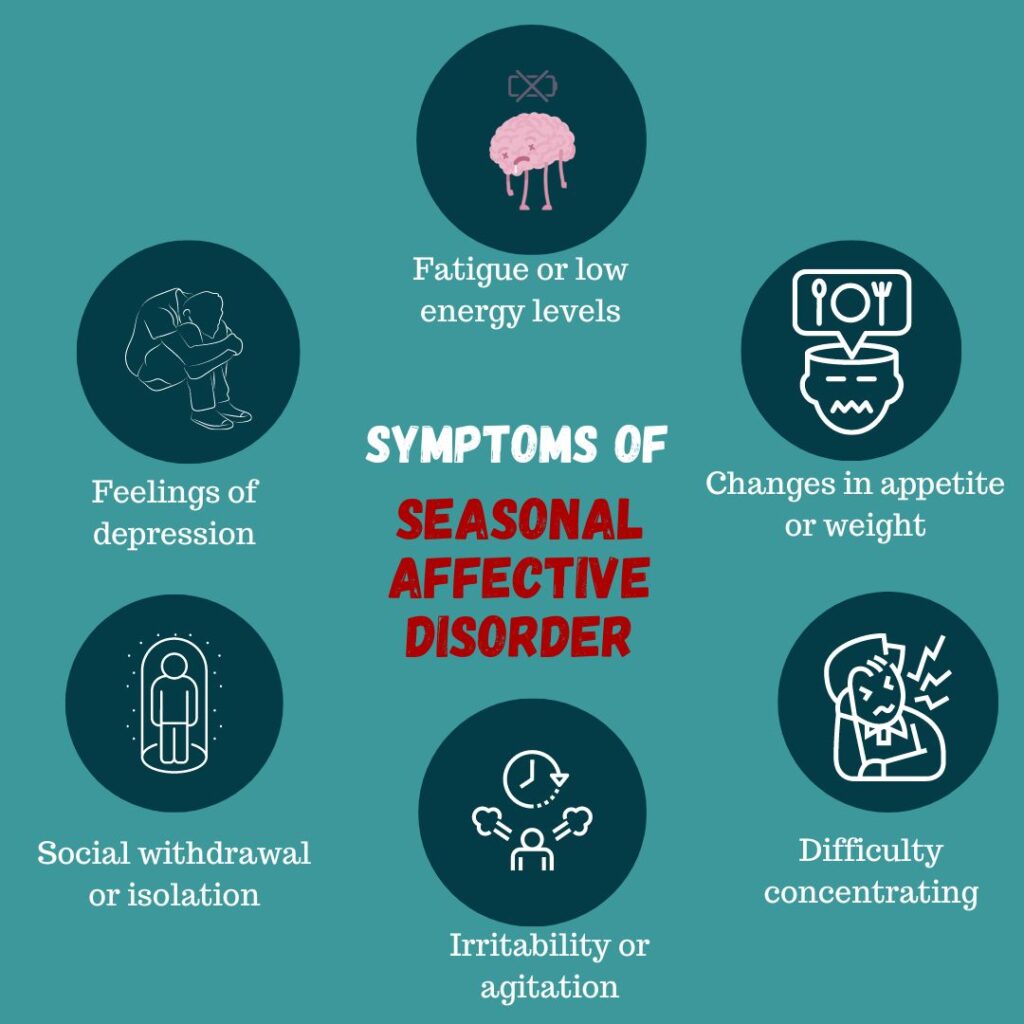
Recognizing SAD Symptoms: Seasonal Triggers and Psychological Impact
The clinical features of SAD mirror those of major depression but occur cyclically with seasonal onset. Patients often report a predictable worsening of symptoms at the same time each year.
Common Symptoms
- Persistent low mood
- Hypersomnia
- Anhedonia (loss of interest)
- Fatigue and low energy
- Difficulty concentrating
- Social withdrawal
- Increased appetite, especially for carbohydrates
- Weight gain
Summer-Pattern SAD Variations
- Insomnia
- Agitation
- Weight loss
- Anxiety
Diagnostic Criteria and Assessment Tools
Diagnosis of SAD is primarily clinical and follows the criteria established in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Diagnostic Requirements
- Depressive episodes occurring at specific times of the year for at least two consecutive years
- Full remission during other seasons
- Greater frequency of seasonal episodes than non-seasonal depressive episodes
Assessment Methods
- Structured Clinical Interview for DSM (SCID)
- Seasonal Pattern Assessment Questionnaire (SPAQ)
- Patient Health Questionnaire (PHQ-9) adapted for seasonality
Light Therapy for Seasonal Affective Disorder
Light therapy is the first-line treatment for winter-pattern SAD. It involves daily exposure to bright artificial light that mimics natural sunlight, aiming to recalibrate circadian rhythms.
Protocol
- Intensity: 10,000 lux
- Duration: 20–30 minutes daily
- Timing: Morning exposure most effective
- Device: Full-spectrum light box with UV filtering
Efficacy and Considerations
- Improvement often observed within 1–2 weeks
- Side effects may include eye strain, headache, and irritability
- Contraindicated in patients with bipolar disorder due to risk of mania
Pharmacologic Treatment Options
In cases of moderate to severe SAD or when light therapy is insufficient, antidepressant therapy may be warranted.
Selective Serotonin Reuptake Inhibitors (SSRIs)
- Fluoxetine, Sertraline, Paroxetine
- Effective in reducing symptoms and preventing recurrence
Bupropion XL
- Approved by FDA for SAD prevention
- Initiated in early fall to mitigate onset
Treatment Strategy
- Minimum 3–6 months during high-risk seasons
- Gradual discontinuation in spring if remission achieved
Psychotherapy and Cognitive-Behavioral Approaches
Cognitive Behavioral Therapy (CBT) has proven efficacy in managing SAD, particularly in addressing maladaptive thoughts and behaviors linked to the seasonal pattern.
Core CBT Components
- Behavioral activation
- Cognitive restructuring
- Relapse prevention planning
Advantages Over Light Therapy
- Lower relapse rates post-treatment
- Focus on long-term coping strategies
Lifestyle Adjustments and Preventive Measures
Environmental and behavioral interventions can significantly reduce the severity of seasonal depressive symptoms.
Recommended Strategies
- Maximize sunlight exposure: Outdoor activities during daylight
- Maintain consistent sleep schedule: Support circadian stability
- Physical exercise: Enhances endorphin release
- Vitamin D supplementation: May address deficiency linked to mood regulation
- Mindfulness and stress management: Supports emotional resilience
Differential Diagnosis and Comorbid Conditions
SAD must be differentiated from other psychiatric and physiological conditions to ensure accurate treatment.
| Condition | Key Differentiators |
|---|---|
| Major Depressive Disorder | Non-seasonal pattern |
| Bipolar Disorder | Presence of manic or hypomanic episodes |
| Hypothyroidism | Fatigue, weight gain, and depression, but confirmed via TSH testing |
| Atypical Depression | Similar symptoms, but not seasonally patterned |
Prognosis and Long-Term Outlook
The prognosis for SAD is generally favorable with appropriate management. Most individuals experience substantial symptom relief through a combination of light therapy, medications, and behavioral strategies. However, recurrence is common without preventive measures.
Recurrence Risk Factors
- Family history of mood disorders
- Lack of sunlight exposure
- Comorbid anxiety or depression
Ongoing Research and Future Perspectives
- Chronotherapy: Exploration of melatonin agonists and circadian realignment techniques
- Genetic Studies: Identification of biomarkers associated with SAD susceptibility
- Personalized Light Therapy: Adjustments in timing and spectrum for optimized outcomes
- Digital CBT Platforms: Expanding accessibility through teletherapy and app-based interventions
Seasonal Affective Disorder is a well-defined clinical entity characterized by recurrent depressive episodes aligned with seasonal light variation. Effective management relies on early recognition, evidence-based therapies such as light therapy and antidepressants, and supportive behavioral modifications. Continued research into circadian biology and digital therapeutic interventions holds promise for enhanced precision in treatment.

