Sclerotherapy remains a critical intervention for managing esophageal varices, particularly in patients with portal hypertension. However, while effective, the procedure carries a risk of mucosal complications, including sclerotherapy-induced mucositis. This condition, characterized by inflammation and damage to the esophageal mucosa, can significantly impact patient recovery and overall treatment success. A thorough understanding of its etiology, clinical presentation, diagnostic modalities, and therapeutic strategies is essential for effective management.
Pathophysiology of Sclerotherapy-Induced Mucositis
Sclerotherapy-induced mucositis arises due to the caustic effects of sclerosant agents on the esophageal mucosa. The primary mechanism involves direct chemical injury to the epithelial lining, initiating a cascade of inflammatory responses that result in mucosal edema, erythema, and eventual ulceration in severe cases.
Commonly used sclerosants such as ethanolamine oleate, sodium tetradecyl sulfate, and polidocanol act by denaturing proteins and obliterating vascular endothelium. However, their diffusion into adjacent mucosal tissue can trigger acute mucosal inflammation and necrosis, particularly when injection techniques are suboptimal or repeated too frequently.
Risk Factors Contributing to Mucosal Injury
The development of mucositis post-sclerotherapy is influenced by several patient-related and procedural factors:
- High Concentration or Volume of Sclerosant: Overexposure increases the likelihood of collateral tissue injury.
- Frequent Sessions: Repeated sclerotherapy within short intervals limits mucosal healing time.
- Injection Technique: Intra-variceal versus paravariceal injection accuracy significantly affects mucosal exposure.
- Underlying Mucosal Vulnerability: Patients with preexisting esophageal inflammation, malnutrition, or immune suppression are more susceptible.
- Concurrent Therapies: Radiation, chemotherapy, or NSAIDs can exacerbate mucosal damage.
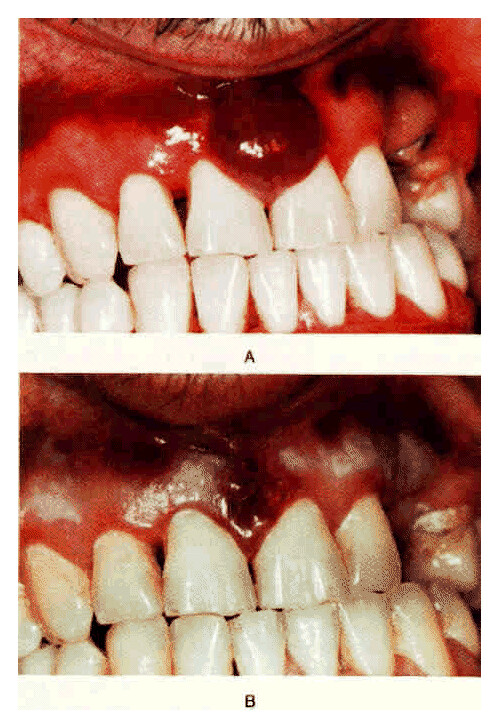
Clinical Manifestations of Sclerotherapy-Induced Mucositis
Mucositis typically develops within days of sclerotherapy and varies in severity. The clinical presentation includes:
- Odynophagia: Painful swallowing is the hallmark symptom.
- Dysphagia: Patients may report difficulty or obstruction in food passage.
- Retrosternal Discomfort: Burning or aching behind the sternum.
- Hypersalivation or Metallic Taste: Due to inflamed mucosa and altered secretion.
- Fever or Malaise: Indicative of secondary infection or systemic inflammatory response.
In advanced cases, mucositis may progress to ulceration, bleeding, or stricture formation if not promptly addressed.
Diagnostic Evaluation of Sclerotherapy-Induced Mucositis
Accurate diagnosis relies on endoscopic visualization and patient history. The key diagnostic steps include:
1. Esophagogastroduodenoscopy (EGD)
- Direct visualization of erythema, friability, edema, ulceration.
- Enables biopsy if differentiation from infectious or neoplastic lesions is needed.
2. Histopathological Examination
- Reveals epithelial necrosis, inflammatory infiltrate, and ulcerative changes.
- Helps distinguish mucositis from eosinophilic or infectious esophagitis.
3. Radiologic Imaging
- Contrast-enhanced studies may identify strictures or perforations in complicated cases.
4. Clinical Correlation
- Assessment of onset relative to sclerotherapy session timing strengthens diagnosis.
Management and Treatment of Sclerotherapy-Induced Mucositis
Treatment aims to reduce inflammation, promote mucosal healing, and manage symptoms. A multi-modal approach is often required.
Pharmacological Management
- Proton Pump Inhibitors (PPIs): Reduce acid exposure to facilitate mucosal repair.
- Sucralfate Suspension: Forms a protective barrier over inflamed mucosa, promoting epithelial healing.
- Topical Anesthetics (e.g., viscous lidocaine): Alleviate odynophagia.
- Antibiotics: Used empirically if secondary infection is suspected.
- Corticosteroids: May be considered in severe, refractory inflammation but require caution due to ulcer risk.
Nutritional Support
- Soft or Liquid Diets: Minimize mechanical trauma to the esophageal lining.
- Parenteral Nutrition: Reserved for severe cases where oral intake is not tolerated.
Procedural Interventions
- Endoscopic Dilation: For post-inflammatory strictures.
- Repeat Endoscopy: To monitor healing progression or address bleeding.
Preventive Strategies for Mucosal Complications
Prevention of sclerotherapy-induced mucositis hinges on proper technique and patient selection:
- Optimal Injection Technique: Ensuring accurate intra-variceal delivery minimizes sclerosant extravasation.
- Spacing Treatment Intervals: Allowing time for mucosal recovery between sessions reduces cumulative injury.
- Agent Selection and Dosage Adjustment: Using the lowest effective concentration mitigates chemical trauma.
- Patient Preparation: Managing reflux, avoiding NSAIDs, and ensuring good nutritional status prior to treatment.
- Post-Procedural Monitoring: Early symptom recognition can prompt swift intervention.
Complications of Untreated Mucositis
Failure to manage mucositis effectively may lead to serious outcomes, including:
- Esophageal Ulceration and Bleeding
- Stricture Formation with Chronic Dysphagia
- Superimposed Fungal or Bacterial Infections
- Perforation (rare but life-threatening)
Such complications often necessitate more invasive interventions and prolong hospitalization.
Prognosis and Follow-Up
With early identification and appropriate therapy, most cases of sclerotherapy-induced mucositis resolve within days to weeks. Regular follow-up with endoscopy may be necessary in recurrent cases or if complications are suspected.
Sclerotherapy-induced mucositis is a clinically significant adverse effect of variceal therapy that demands vigilant recognition and management. Adhering to best practices in sclerotherapy technique, coupled with timely therapeutic interventions, can mitigate the impact of mucosal injury and preserve esophageal function. Continuous advancements in endoscopic protocols and pharmacologic support further enhance our ability to prevent and resolve this complication effectively.