Scleroderma renal crisis (SRC) is an acute, life-threatening complication of systemic sclerosis (scleroderma) characterized by rapid onset of severe hypertension and acute kidney injury. It represents one of the most urgent medical emergencies in scleroderma patients, primarily affecting those with diffuse cutaneous systemic sclerosis.
Clinical Presentation and Symptoms of SRC
SRC typically presents abruptly and can rapidly progress if not promptly diagnosed and treated. The hallmark features include:
- Sudden onset of malignant hypertension
- Acute kidney injury (elevated serum creatinine, reduced glomerular filtration rate)
- Headache, visual disturbances, or seizures (due to hypertensive encephalopathy)
- Proteinuria and hematuria
- Microangiopathic hemolytic anemia (MAHA)
- Oliguria or anuria in severe cases
Additional Warning Signs
- New-onset hypertension in a patient with previously normal blood pressure
- Retinopathy with cotton wool spots or hemorrhages
- Thrombocytopenia and elevated lactate dehydrogenase (LDH)
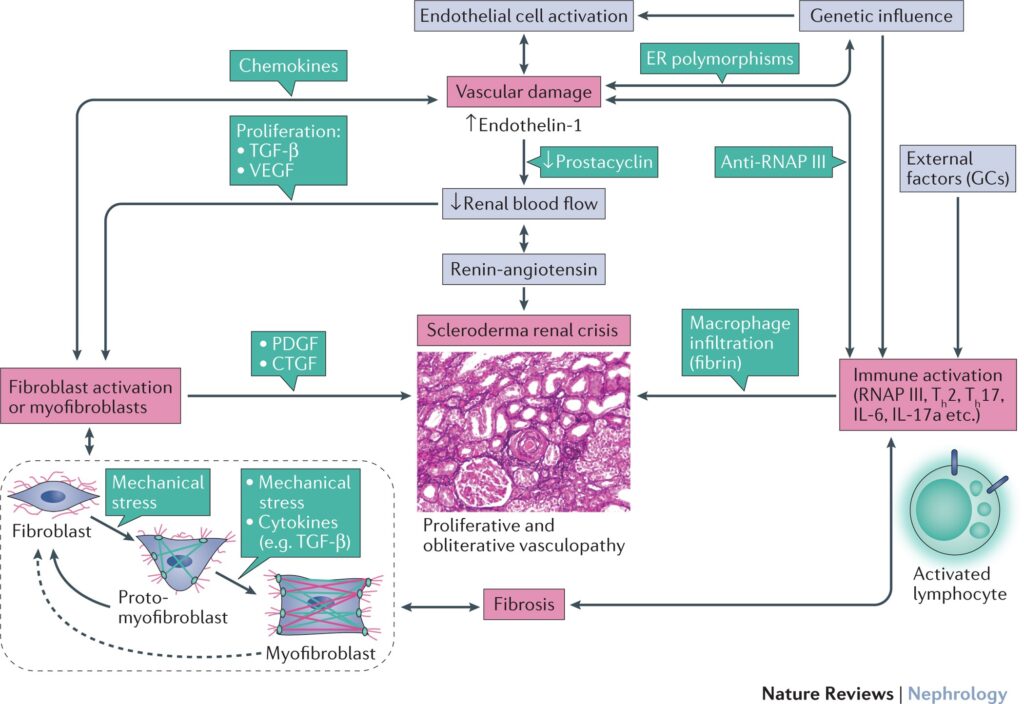
Pathophysiology of Scleroderma Renal Crisis
SRC results from vascular endothelial injury, leading to narrowing of renal arteries, ischemia, and activation of the renin-angiotensin system.
This vicious cycle perpetuates worsening kidney function, making early therapeutic interruption critical.
Risk Factors and Predisposing Conditions
Several factors increase the likelihood of SRC, most notably:
- Diffuse cutaneous systemic sclerosis (especially within the first 5 years of diagnosis)
- Presence of anti-RNA polymerase III antibodies
- Rapid skin thickening
- High-dose corticosteroid use
- Previous hypertensive episodes
Patients with these risk factors must be closely monitored for early detection.
Diagnostic Evaluation of SRC
Timely and accurate diagnosis is vital. Diagnosis is based on clinical features, laboratory studies, and exclusion of other causes of acute kidney injury.
Diagnostic Criteria
- Abrupt onset of hypertension (≥150/85 mmHg)
- Rising serum creatinine and/or decreased urine output
- Presence of proteinuria, hematuria, or active urinary sediment
- Peripheral blood smear showing schistocytes (MAHA)
- Thrombocytopenia
- Elevated LDH and reticulocyte count
Supporting Tests
- Renal ultrasound to rule out obstruction
- Fundoscopy to assess hypertensive retinopathy
- Autoantibody panel for anti-RNA polymerase III
- 24-hour blood pressure monitoring
Kidney biopsy is rarely needed but may show onion-skin arteriolar lesions in uncertain cases.
Management and Treatment of Scleroderma Renal Crisis
First-Line Therapy: ACE Inhibitors
Angiotensin-converting enzyme inhibitors (ACEIs), especially captopril, remain the cornerstone of SRC treatment due to their ability to:
- Lower blood pressure
- Block renin-angiotensin system
- Reduce glomerular injury
- Preserve renal perfusion
Initiation should occur immediately upon suspicion, even before creatinine levels rise significantly.
Captopril Dosing Strategy
- Start at low dose (e.g., 12.5–25 mg three times daily)
- Titrate up as tolerated
- Monitor serum potassium and renal function closely
Adjunctive Measures
- Avoid high-dose corticosteroids if possible
- Discontinue nephrotoxic agents
- Monitor urine output and blood pressure hourly
- Dialysis may be required in severe cases; however, some patients recover kidney function with continued ACEI therapy
Prognosis and Long-Term Outcomes
Before the advent of ACE inhibitors, SRC carried a mortality rate exceeding 75%. With early diagnosis and proper therapy, outcomes have improved significantly.
Prognostic Indicators
| Favorable Outcome Factors | Poor Prognosis Indicators |
|---|---|
| Early ACEI initiation | Delayed or no treatment |
| Anti-centromere antibodies | Anti-RNA polymerase III antibodies |
| Controlled hypertension | Severe hypertensive crisis |
| Partial kidney function recovery | Dialysis dependence after 12 months |
Even in dialysis-dependent patients, recovery of renal function can occur after prolonged ACEI therapy, and kidney transplantation is an option for non-recovering cases.
Prevention Strategies for High-Risk Patients
While not all SRC cases are preventable, risk can be minimized by:
- Avoiding high-dose steroids, particularly in diffuse cutaneous scleroderma
- Regular monitoring of blood pressure and renal function
- Screening for anti-RNA polymerase III antibodies
- Educating patients on early warning signs
- Maintaining close surveillance during the first five years of systemic sclerosis
Patient Monitoring and Follow-Up
Long-term management involves:
- Lifelong use of ACE inhibitors if tolerated
- Routine monitoring of:
- Blood pressure
- Serum creatinine
- Electrolytes (especially potassium)
- Urinalysis for proteinuria
- Periodic echocardiography and pulmonary assessments to evaluate systemic sclerosis complications
Patients should be co-managed by rheumatologists, nephrologists, and primary care providers for optimal outcomes.
Scleroderma renal crisis is a critical complication of systemic sclerosis that demands immediate recognition and intervention. Prompt administration of ACE inhibitors significantly reduces mortality and preserves renal function. Clinicians must maintain vigilance in high-risk patients and educate them on the importance of early symptom reporting. With appropriate management, survival and quality of life for those affected can be substantially improved.