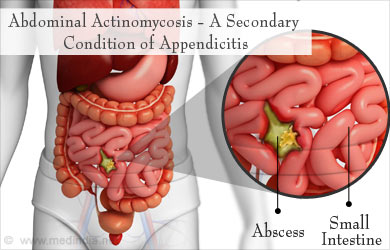
Abdominal actinomycosis is a rare, chronic bacterial infection caused by the Actinomyces species, predominantly Actinomyces israelii. This condition typically presents as a slowly progressing disease characterized by abscess formation, fibrosis, and sinus tract development. Understanding its clinical manifestations, diagnostic approaches, and treatment modalities is crucial for effective management.
Etiology and Pathophysiology of Abdominal Actinomycosis
Actinomyces are anaerobic or facultative anaerobic Gram-positive bacteria that reside as commensals in the oral cavity, gastrointestinal tract, and female genital tract. Disruption of mucosal barriers, such as from surgical procedures, trauma, or gastrointestinal perforations, often provides an entry point for these bacteria, leading to localized infections.
In the abdomen, actinomycosis frequently affects the ileocecal region but can involve any part of the gastrointestinal tract. The infection progresses insidiously, mimicking malignancies or other chronic inflammatory conditions. Actinomyces form colonies embedded in granules known as sulfur granules, which are pathognomonic for the disease.
Risk Factors for Abdominal Actinomycosis
Several factors predispose individuals to abdominal actinomycosis, including:
- Surgical Interventions: Abdominal surgeries such as appendectomies or cesarean sections.
- Intrauterine Devices (IUDs): Prolonged use has been linked to pelvic and abdominal actinomycosis.
- Gastrointestinal Disorders: Conditions like diverticulitis, perforated ulcers, or Crohn’s disease increase susceptibility.
- Immunosuppression: Conditions such as diabetes or therapies like chemotherapy.
Clinical Presentation
The nonspecific symptoms and slow progression of abdominal actinomycosis often lead to delayed diagnosis. Common signs and symptoms include:
- Abdominal Pain: Persistent and poorly localized.
- Fever: Low-grade, often accompanying other systemic signs.
- Weight Loss: Unintentional and gradual.
- Palpable Mass: Mimicking malignancies.
- Sinus Tracts: Draining pus externally or internally into other organs.
Diagnostic Approach
Diagnosing abdominal actinomycosis requires a combination of clinical suspicion, imaging studies, and microbiological confirmation.
Imaging Studies
- Ultrasound: Identifies masses, abscesses, or fluid collections.
- Computed Tomography (CT): Offers detailed visualization of lesions, including their extent and relation to surrounding structures.
- Magnetic Resonance Imaging (MRI): Useful for soft tissue assessment and differentiation from malignancies.
Microbiological Examination
- Specimen Collection: Samples from abscesses, biopsies, or sinus tract discharges.
- Microscopy: Identifies sulfur granules and Gram-positive branching filaments.
- Culture: Requires anaerobic conditions; growth is slow, often taking up to 2 weeks.
Histopathological Examination
Histology often reveals chronic inflammatory changes, granulomatous reactions, and the presence of sulfur granules.
Differential Diagnosis
The clinical presentation of abdominal actinomycosis overlaps with several conditions, necessitating careful differentiation from:
- Gastrointestinal Malignancies: Particularly colorectal cancer.
- Crohn’s Disease: Chronic inflammatory features.
- Tuberculosis: Abdominal TB can mimic actinomycosis.
- Other Infections: Such as nocardiosis or fungal infections.
Treatment Modalities
Effective management of abdominal actinomycosis requires a combination of prolonged antibiotic therapy and surgical intervention in selected cases.
Antibiotic Therapy
- Penicillin: The cornerstone of treatment, administered intravenously for 4-6 weeks, followed by oral therapy for 6-12 months.
- Alternatives: Doxycycline, erythromycin, or clindamycin for penicillin-allergic patients.
Surgical Intervention
- Indicated for extensive abscesses, fistulas, or intestinal obstruction.
- Aims to remove necrotic tissue and establish drainage.
Prognosis and Complications
With timely diagnosis and appropriate treatment, the prognosis is favorable. However, delayed treatment can result in significant complications, including:
- Chronic Sinus Tracts: Persistent draining tracts.
- Fistula Formation: Between abdominal organs or to the skin.
- Sepsis: From systemic spread.
Prevention and Awareness
Raising awareness about abdominal actinomycosis among healthcare providers is essential for early recognition and management. Preventive strategies include:
- Proper surgical technique and post-operative care.
- Monitoring for infections in high-risk individuals.
- Regular follow-ups for patients with IUDs or gastrointestinal diseases.
Abdominal actinomycosis, though rare, poses a diagnostic challenge due to its nonspecific presentation and resemblance to other conditions. Clinicians should maintain a high index of suspicion in patients with chronic abdominal symptoms, especially those with predisposing factors. Early diagnosis and a multidisciplinary approach involving antibiotics and, when necessary, surgical management are key to improving outcomes.