Schizoaffective disorder is a complex and chronic psychiatric condition characterized by a combination of symptoms seen in both schizophrenia and mood disorders (either depression or bipolar disorder). Individuals with schizoaffective disorder experience episodes of psychosis—including hallucinations and delusions—alongside mood disturbances. It is a unique diagnosis, distinct from schizophrenia or bipolar disorder alone, and requires careful clinical evaluation.
Classification: Bipolar Type vs. Depressive Type
Schizoaffective disorder is divided into two subtypes based on the nature of the mood episodes that accompany psychotic symptoms:
- Bipolar Type: Involves episodes of mania and sometimes major depression.
- Depressive Type: Involves only major depressive episodes.
This classification is essential for tailoring treatment strategies, as the management approach for mood symptoms varies between the two.
Causes and Risk Factors
While the exact cause of schizoaffective disorder remains unknown, it is likely the result of an interplay between genetic, neurobiological, and environmental factors:
- Genetics: A family history of schizophrenia, bipolar disorder, or depression increases risk.
- Brain Structure and Chemistry: Abnormalities in neurotransmitter systems (especially dopamine and serotonin) and brain imaging studies showing structural differences may contribute.
- Stressful Life Events: Trauma, abuse, or significant life stressors may act as triggers.
- Substance Abuse: Drugs such as LSD, cocaine, or amphetamines can induce symptoms or exacerbate the condition.
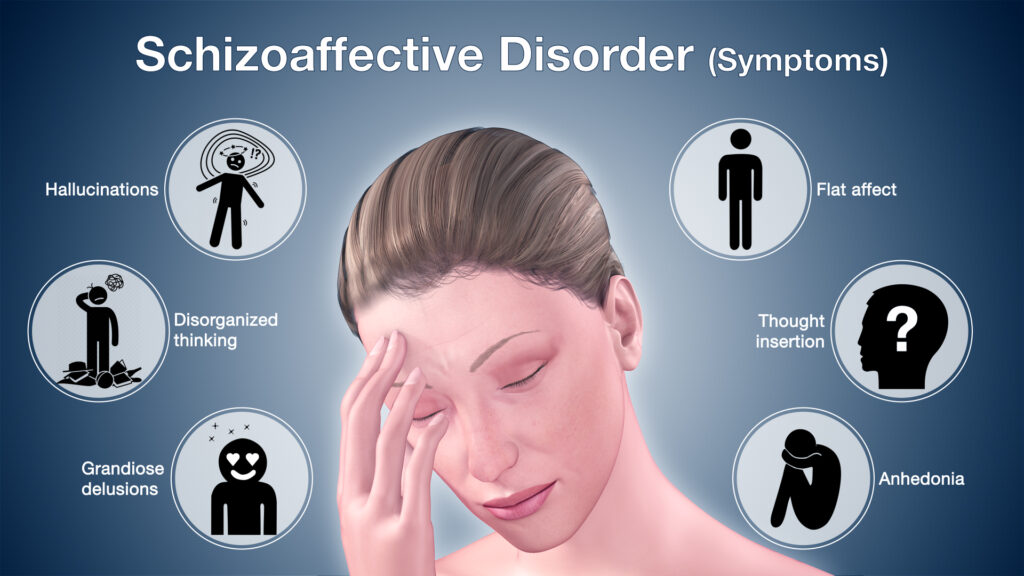
Key Symptoms of Schizoaffective Disorder
Symptoms typically occur in phases, often fluctuating over time. They can be broadly categorized as follows:
Psychotic Symptoms
- Hallucinations: Most often auditory (hearing voices)
- Delusions: Strongly held false beliefs (e.g., paranoia, grandiosity)
- Disorganized Thinking: Impaired ability to organize thoughts or communicate effectively
- Catatonia: Physical immobility or excessive movement without purpose
Mood Symptoms
- Depressive Symptoms:
- Persistent sadness
- Anhedonia (loss of interest in previously enjoyable activities)
- Fatigue
- Suicidal ideation
- Manic Symptoms (in bipolar type):
- Inflated self-esteem or grandiosity
- Decreased need for sleep
- Pressured speech
- Risky behaviors (e.g., spending sprees, impulsive decisions)
Functional Impairment
Schizoaffective disorder significantly disrupts daily functioning, affecting work, relationships, self-care, and overall quality of life.
Diagnostic Criteria and Evaluation
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) outlines specific criteria for diagnosing schizoaffective disorder:
Diagnostic Tools
- Clinical Interview: A comprehensive psychiatric assessment
- Psychiatric Rating Scales: PANSS (Positive and Negative Syndrome Scale), Hamilton Depression Rating Scale
- Laboratory Tests and Imaging: Rule out organic or substance-induced psychosis
- Longitudinal Observation: Necessary to differentiate from schizophrenia or mood disorder with psychotic features
Schizoaffective Disorder vs. Similar Conditions
| Condition | Psychosis | Mood Episodes | Distinction |
|---|---|---|---|
| Schizoaffective Disorder | Yes | Yes | Both symptoms occur independently |
| Schizophrenia | Yes | Rare/minimal | Mood symptoms are brief or absent |
| Bipolar Disorder w/ Psychosis | Yes | Yes | Psychosis occurs only during mood episodes |
| Major Depression w/ Psychosis | Yes | Yes | Psychosis always tied to depression |
Treatment and Management
Treatment of schizoaffective disorder typically involves a multimodal approach, integrating pharmacologic therapy, psychotherapy, and psychosocial support.
Pharmacologic Treatment
- Antipsychotics: To manage psychosis
- Examples: Risperidone, Olanzapine, Paliperidone (FDA-approved for schizoaffective disorder)
- Mood Stabilizers (for bipolar type)
- Lithium, Valproate, Carbamazepine
- Antidepressants (for depressive type)
- SSRIs or SNRIs under supervision to prevent manic switch
Psychotherapy
- Cognitive Behavioral Therapy (CBT): Helps patients challenge delusions, improve mood regulation, and enhance coping mechanisms
- Family Therapy: Supports family members and educates about the disorder
- Social Skills Training: Addresses functional impairments and social isolation
Lifestyle and Supportive Care
- Stable routine and sleep hygiene
- Peer support groups and vocational rehabilitation
- Case management for housing, employment, and community reintegration
Prognosis and Long-Term Outlook
The course of schizoaffective disorder is variable. Some individuals respond well to treatment and achieve long periods of stability, while others experience recurrent episodes. Early diagnosis, medication adherence, and comprehensive psychosocial support are key predictors of better outcomes.
Complications from untreated or poorly managed schizoaffective disorder may include:
- Suicidal behavior
- Social withdrawal
- Homelessness
- Substance abuse
- Co-occurring medical conditions
Living with Schizoaffective Disorder: Coping and Advocacy
Effective coping involves:
- Medication adherence
- Monitoring triggers and early signs of relapse
- Building a support system
- Accessing professional help promptly
Mental health advocacy plays a vital role in reducing stigma, ensuring policy support, and improving access to care. Increasing awareness can empower individuals and communities to foster inclusive environments for those living with schizoaffective disorder.
Schizoaffective disorder is a serious but manageable condition when approached with informed, integrated, and compassionate care. Through early detection, individualized treatment, and ongoing support, individuals affected by schizoaffective disorder can achieve meaningful recovery and improved quality of life.

