Scabies is a highly contagious skin infestation caused by the Sarcoptes scabiei var. hominis mite. It leads to intense pruritus, particularly at night, and is transmitted through prolonged skin-to-skin contact. Globally, scabies affects over 200 million people at any time and remains a significant public health burden, especially in crowded living environments and among vulnerable populations.

Causative Agent: Sarcoptes scabiei Mite
Scabies is caused by the female Sarcoptes scabiei mite, which burrows into the stratum corneum of human skin to lay eggs.
- Adult female size: ~0.3–0.4 mm
- Lifecycle: ~10–17 days
- Survival off host: Up to 2–3 days on bedding or clothing
Transmission of Scabies
Scabies spreads predominantly through prolonged direct skin-to-skin contact, making it highly transmissible among household members, sexual partners, and in institutional settings.
Primary Modes of Transmission:
- Direct skin contact: Most common route
- Fomites: Bedding, clothing, and towels (more relevant in crusted scabies)
- Sexual contact: Especially in young adults
Scabies is not a sign of poor hygiene, and anyone can be infected regardless of cleanliness.
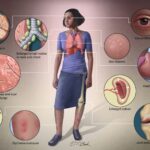
Clinical Manifestations of Scabies
General Symptoms
- Intense itching, especially nocturnal
- Erythematous papules and burrows
- Secondary bacterial infection due to scratching
Common Sites of Infestation
| Affected Area | Description |
|---|---|
| Interdigital spaces | Webs between fingers |
| Wrists and elbows | Flexor surfaces |
| Axillae | Warm, moist skin folds |
| Waist and buttocks | Common in adults |
| Genital area | Common in men |
| Areolae and breasts | Common in women |
Burrows
Thin, grayish-white, serpiginous lines representing mite tunnels; most diagnostic of scabies.
Variants of Scabies
1. Classic Scabies
- Most common form
- Presents with burrows and intense pruritus
2. Nodular Scabies
- Hypersensitivity reaction
- Itchy nodules, often on genitalia or axillae
3. Crusted (Norwegian) Scabies
- Severe, highly contagious form
- Thick crusts teeming with mites
- Occurs in immunocompromised individuals
4. Infantile Scabies
- Affects palms, soles, scalp
- Vesicles and pustules more common
Diagnosis of Scabies
Clinical Diagnosis
- Based on history (pruritus, contact) and characteristic lesions
- Family members often exhibit similar symptoms
Confirmatory Methods
- Skin scraping: Microscopic identification of mites, eggs, or fecal pellets
- Dermatoscopy: “Jet with contrail” sign indicating burrow
- Adhesive tape test: Collects superficial mites for microscopy
Differential Diagnoses
- Atopic dermatitis
- Contact dermatitis
- Lichen planus
- Folliculitis
- Insect bites
Differentiation is essential to avoid misdiagnosis and inappropriate treatment.
Treatment Protocols for Scabies
Prompt treatment is vital to relieve symptoms and prevent spread.
First-Line Treatments
- Permethrin 5% cream: Apply from neck to toes, leave for 8–14 hours
- Oral ivermectin: 200 mcg/kg as a single dose, repeated in 7–14 days
Alternative Treatments
- Benzyl benzoate 25%
- Sulfur 5–10% in petrolatum (infants and pregnant women)
- Crotamiton 10% lotion
Management of Crusted Scabies
- Combination therapy: Oral ivermectin + topical permethrin
- Isolation and environmental decontamination required
Environmental Control and Prevention
Preventing Reinfestation
- Wash all clothing, bedding, towels in hot water (>50°C)
- Items that cannot be washed should be sealed for 72 hours
- Treat all close contacts, even if asymptomatic
Institutional Outbreak Control
- Mass treatment in nursing homes, prisons
- Staff education and surveillance
Complications of Untreated Scabies
- Secondary bacterial infection: Impetigo, cellulitis
- Post-scabetic pruritus: Itch may persist after mite eradication
- Chronic eczema
- Glomerulonephritis: Post-streptococcal infection risk in children
Prognosis and Follow-Up
With effective treatment and adherence to environmental measures, the prognosis is excellent. Itching may continue for several weeks due to a hypersensitivity reaction. Re-treatment may be necessary in persistent or reinfected cases.
Follow-Up Recommendations
- Re-examine 2–4 weeks post-treatment
- Repeat treatment if live mites or new lesions are observed
- Assess close contacts for signs of infestation
Public Health Considerations
Scabies is classified as a Neglected Tropical Disease (NTD) by the WHO due to its high global burden and potential for epidemics. Efforts are ongoing to improve community-based management and access to effective treatments in endemic regions.
Summary Table: Key Facts about Scabies
| Feature | Description |
|---|---|
| Causative agent | Sarcoptes scabiei var. hominis |
| Transmission | Direct skin contact, less commonly fomites |
| Incubation period | 2–6 weeks (shorter in re-infestation) |
| Diagnostic hallmark | Burrows, pruritus, positive skin scraping |
| First-line treatment | Permethrin 5% cream, oral ivermectin |
| Contagious? | Yes, highly |
| At-risk populations | Children, elderly, immunocompromised |
Scabies, though curable, requires timely recognition, targeted treatment, and comprehensive contact tracing to prevent recurrent outbreaks. Clinicians and public health authorities must remain vigilant in endemic and institutional settings to minimize morbidity and prevent complications.