Sarcoidosis is a chronic granulomatous disease of unknown etiology that predominantly affects the lungs and lymphatic system, though it can involve virtually any organ. Characterized by the formation of non-caseating granulomas, this condition presents with a wide spectrum of clinical manifestations, ranging from asymptomatic to life-threatening.
The disease affects individuals of all ethnicities and ages but is most common in adults between 20 and 40 years. Its variable presentation makes early detection and management essential for optimal outcomes.
Etiology and Risk Factors of Sarcoidosis
While the precise cause remains unknown, sarcoidosis is believed to result from an exaggerated immune response to unidentified environmental antigens in genetically susceptible individuals.
Suspected Triggers
- Infectious agents (e.g., Mycobacterium spp., Propionibacterium acnes)
- Occupational exposures (e.g., beryllium, mold, dust)
- Autoimmune activation in genetically predisposed hosts
Risk Factors
- Family history of sarcoidosis
- African American or Scandinavian descent
- Female sex (slightly higher incidence)
- Occupations with exposure to inorganic dusts or bioaerosols
Pathophysiology of Sarcoidosis
The hallmark of sarcoidosis is non-caseating granulomatous inflammation. This immune reaction is driven by T-helper (CD4+) lymphocytes, macrophages, and cytokines like TNF-α and IFN-γ. Granulomas may impair organ function over time.
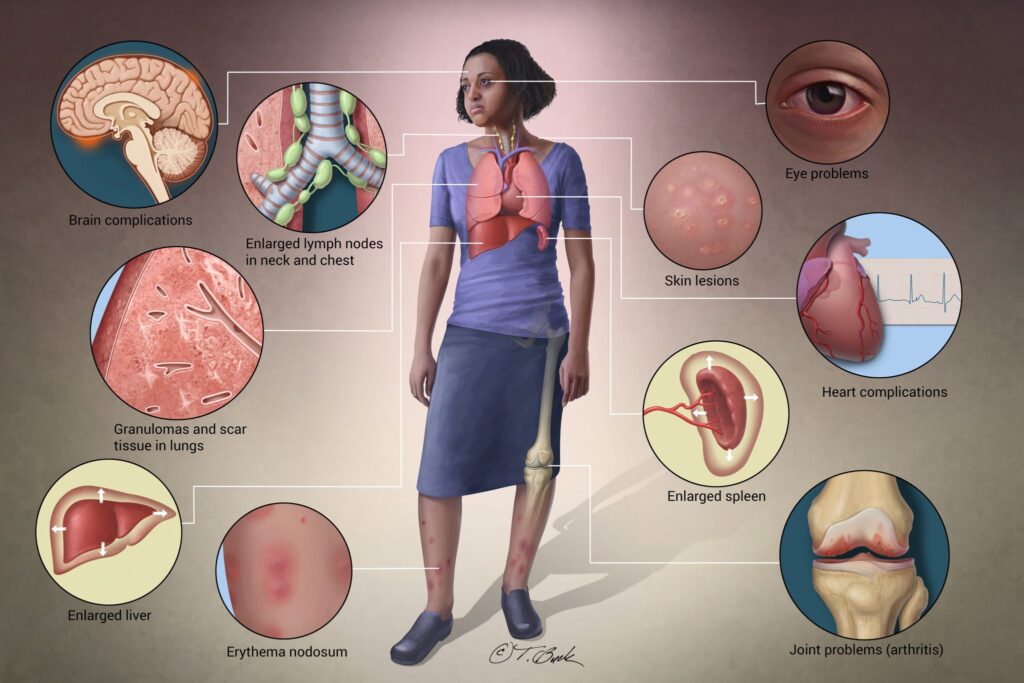
Commonly Affected Organs in Sarcoidosis
Sarcoidosis is a multisystem disorder, and organ involvement may be isolated or diffuse:
| Organ System | Common Manifestations |
|---|---|
| Lungs | Dry cough, dyspnea, chest pain |
| Lymph nodes | Hilar and mediastinal lymphadenopathy |
| Skin | Erythema nodosum, lupus pernio |
| Eyes | Uveitis, conjunctival granulomas |
| Heart | Arrhythmias, cardiomyopathy, heart block |
| Liver and Spleen | Hepatosplenomegaly, abnormal liver enzymes |
| Nervous system | Cranial neuropathy, neurosarcoidosis |
Clinical Presentation of Sarcoidosis
Symptoms depend on the extent and organ involvement. Up to 50% of patients are asymptomatic and diagnosed incidentally via imaging.
General Symptoms
- Fatigue
- Fever
- Weight loss
- Night sweats
Pulmonary Sarcoidosis (most common)
- Persistent dry cough
- Shortness of breath
- Chest tightness or pain
Cutaneous Sarcoidosis
- Erythema nodosum (acute)
- Lupus pernio (chronic)
Ocular Involvement
- Red eyes
- Photophobia
- Visual disturbances
Diagnostic Approach to Sarcoidosis
Diagnosis requires clinical correlation, radiologic findings, and histopathologic confirmation of non-caseating granulomas, while excluding other causes.
Imaging
- Chest X-ray: Bilateral hilar lymphadenopathy (Stage I)
- High-Resolution CT: Parenchymal infiltrates, nodularity, fibrosis
- PET scan: Assess active inflammation and cardiac involvement
Laboratory Tests
- Elevated serum ACE levels (non-specific)
- Hypercalcemia or hypercalciuria
- Elevated ESR, CRP
- Liver function tests
Pulmonary Function Tests
- Restrictive pattern
- Decreased DLCO (diffusing capacity for carbon monoxide)
Biopsy
- Preferred sites: skin, lymph nodes, transbronchial lung biopsy
- Non-caseating granulomas confirm diagnosis
Staging of Pulmonary Sarcoidosis
| Stage | Radiographic Findings |
|---|---|
| I | Bilateral hilar lymphadenopathy |
| II | Hilar lymphadenopathy with pulmonary infiltrates |
| III | Pulmonary infiltrates without lymphadenopathy |
| IV | Pulmonary fibrosis |
Treatment Strategies for Sarcoidosis
Treatment is not required in asymptomatic or mild cases. However, when organ function is at risk or quality of life is impaired, pharmacologic therapy is essential.
First-Line Therapy: Corticosteroids
- Prednisone 20–40 mg/day, tapered over months
- Effective in pulmonary, ocular, and cutaneous involvement
Steroid-Sparing Agents
Used in chronic or steroid-intolerant patients:
- Methotrexate
- Azathioprine
- Leflunomide
- Hydroxychloroquine (cutaneous or hypercalcemia)
Biologic Therapies
- TNF-α inhibitors (e.g., infliximab) for refractory sarcoidosis
Prognosis and Long-Term Outlook
Sarcoidosis has a variable prognosis:
- 2/3 of patients experience spontaneous remission
- Chronic progressive disease occurs in 10–30%
- Pulmonary fibrosis, cardiac sarcoidosis, and neurosarcoidosis are associated with poorer outcomes
Monitoring and Follow-Up
Regular Assessments
- Pulmonary function tests
- Serum calcium and ACE levels
- Ophthalmologic evaluations
- ECG and echocardiography if cardiac involvement suspected
Complications of Sarcoidosis
- Pulmonary fibrosis and respiratory failure
- Cardiac arrhythmias and sudden cardiac death
- Blindness from uveitis
- Renal failure due to hypercalcemia
- Neurosarcoidosis with disabling neurological deficits
Preventive and Supportive Measures
Although sarcoidosis cannot currently be prevented, symptom control and reducing complications remain key.
- Smoking cessation
- Vaccinations (influenza, pneumococcal)
- Bone health monitoring during corticosteroid therapy
- Psychological support for chronic disease management
Sarcoidosis remains a complex and unpredictable inflammatory disease with a broad spectrum of presentations and outcomes. Multidisciplinary management, patient education, and regular follow-up are essential to optimizing long-term health and mitigating complications.