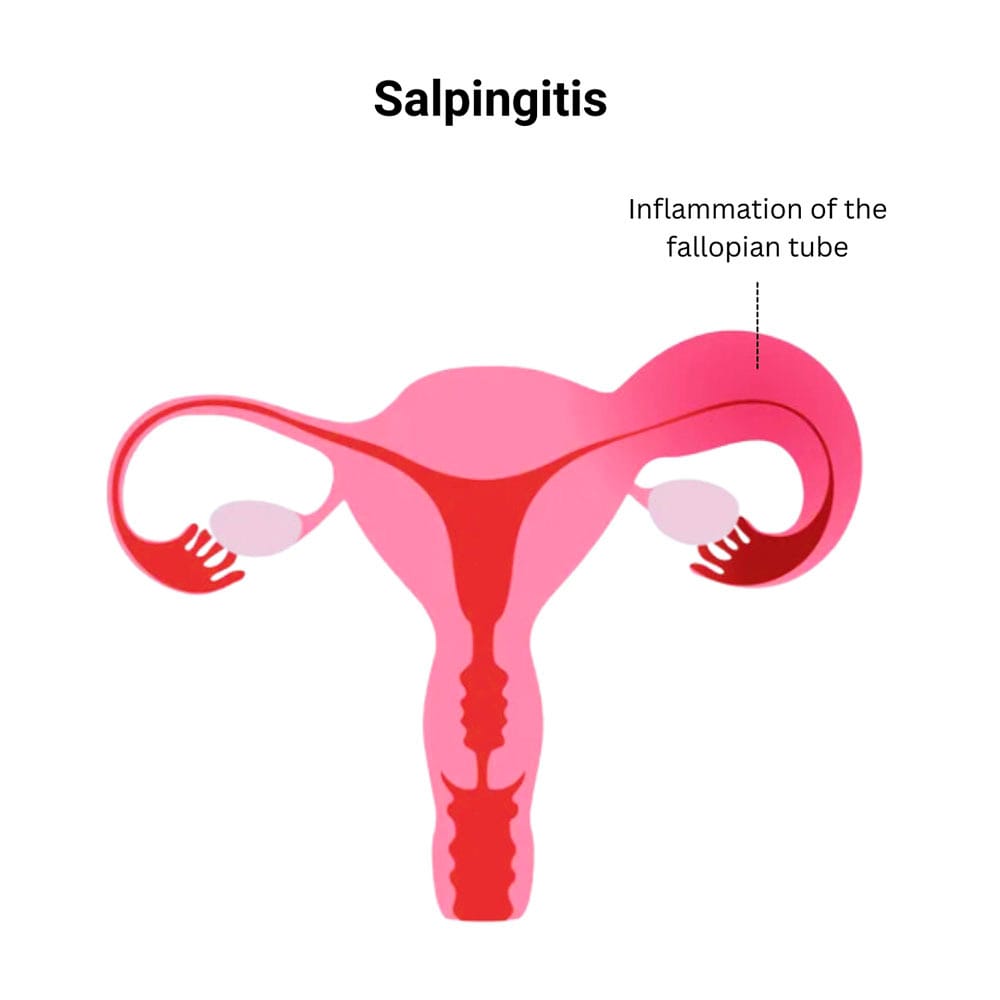
Salpingitis refers to the inflammation of one or both fallopian tubes and represents a significant component of pelvic inflammatory disease (PID). Often caused by ascending bacterial infections, it has the potential to result in chronic pelvic pain, ectopic pregnancy, and infertility if not promptly diagnosed and treated.
This gynecologic condition is especially prevalent among sexually active women of reproductive age and poses considerable public health concerns due to its role in tubal factor infertility.
Causes and Risk Factors of Salpingitis
Bacterial Pathogens Involved
The most common etiologic agents of salpingitis include:
- Neisseria gonorrhoeae
- Chlamydia trachomatis
- Mycoplasma genitalium
- Anaerobes and facultative bacteria from vaginal flora
These pathogens typically ascend from the lower genital tract, especially during menstruation when the cervical barrier is temporarily compromised.
Key Risk Factors
- Multiple sexual partners
- Unprotected intercourse
- History of sexually transmitted infections (STIs)
- Use of intrauterine devices (IUDs)
- Recent gynecologic procedures (e.g., dilation and curettage)
- Previous episodes of PID or salpingitis
Signs and Symptoms of Salpingitis
Clinical presentation can range from mild to severe, with some cases being asymptomatic, especially when caused by Chlamydia trachomatis.
Common Symptoms
- Lower abdominal or pelvic pain
- Fever and chills
- Abnormal vaginal discharge
- Pain during intercourse (dyspareunia)
- Irregular menstrual bleeding
- Painful urination (dysuria)
- Nausea or vomiting in severe cases
Chronic salpingitis may present with persistent pelvic pain, infertility, or menstrual irregularities due to scarring and tubal obstruction.
Pathophysiology of Salpingitis
The progression of infection involves mucosal damage, leukocyte infiltration, and tubal obstruction, increasing the risk for ectopic implantation or permanent tubal occlusion.
Diagnostic Evaluation of Salpingitis
Accurate diagnosis requires a combination of clinical assessment, laboratory testing, and imaging.
Physical Examination
- Lower abdominal tenderness
- Cervical motion tenderness
- Adnexal tenderness
Laboratory Tests
- Complete blood count (CBC): Elevated white blood cell count
- C-reactive protein (CRP), ESR: Indicators of systemic inflammation
- Nucleic acid amplification tests (NAATs): For Chlamydia and Gonorrhea
- Urinalysis and pregnancy test: Rule out differential diagnoses
Imaging Studies
- Transvaginal ultrasound: May reveal dilated fallopian tubes (hydrosalpinx), tubo-ovarian abscess
- MRI or CT: In complex or ambiguous cases
- Laparoscopy (gold standard): Direct visualization and confirmation of tubal inflammation and adhesions
Classification of Salpingitis
Salpingitis can be classified based on duration and severity:
| Type | Description |
|---|---|
| Acute | Sudden onset, severe pain, febrile illness |
| Chronic | Long-standing pain, often after inadequate treatment |
| Subclinical | Asymptomatic, detectable only through screening |
Treatment of Salpingitis
Timely initiation of antibiotic therapy is crucial to prevent complications.
Empirical Antibiotic Regimens
- Ceftriaxone 250–500 mg IM single dose
- Doxycycline 100 mg orally twice daily for 14 days
- Metronidazole 500 mg orally twice daily for 14 days
- Consider IV antibiotics in hospitalized or severe cases (e.g., cefoxitin plus doxycycline)
Supportive Care
- Adequate hydration
- Analgesics for pain relief
- Avoidance of sexual activity until completion of therapy
- Partner notification and treatment to prevent reinfection
Surgical Intervention
Required in cases of:
- Tubo-ovarian abscess
- Refractory symptoms
- Suspected ectopic pregnancy
- Diagnostic uncertainty
Complications of Untreated or Recurrent Salpingitis
Salpingitis is a leading cause of reproductive morbidity:
- Infertility: Due to tubal scarring and blockage
- Ectopic pregnancy: Implantation outside the uterus
- Chronic pelvic pain
- Tubo-ovarian abscess formation
- Peritonitis and sepsis in severe untreated cases
Prevention of Salpingitis
Individual Measures
- Consistent condom use
- Regular STI screening for sexually active individuals
- Prompt treatment of genital infections
- Avoidance of high-risk sexual behaviors
Public Health Interventions
- Sexual health education
- Partner notification and treatment programs
- Vaccination (e.g., HPV vaccine) for broader gynecologic health
- Access to family planning and STI clinics
Salpingitis remains a major contributor to gynecological morbidity, particularly in resource-limited settings. It demands a proactive approach encompassing early diagnosis, appropriate antibiotic therapy, and preventive strategies. Given its implications for fertility and overall reproductive health, awareness and education are as vital as clinical intervention.

