The opioid overdose crisis remains a global public health emergency, driven by both prescription opioids and illicit substances such as fentanyl. To address the escalating rates of opioid-related morbidity and mortality, it is essential to implement robust, evidence-based risk mitigation strategies. These measures encompass preventive interventions, clinical oversight, harm reduction practices, and rapid response systems aimed at saving lives and reducing misuse.
Key Drivers of Opioid Overdose Risk
Effective mitigation begins with understanding the multifactorial causes behind opioid overdose:
- High-dose opioid prescribing
- Concurrent use of sedatives (e.g., benzodiazepines)
- Illicit drug contamination, especially with fentanyl
- Lack of education on opioid risks
- Limited access to treatment for substance use disorder (SUD)
- Barriers to emergency care or naloxone availability
Safe Prescribing Practices and Risk Assessment
Implementing Opioid Prescribing Guidelines
Adherence to clinical guidelines for opioid prescribing is a critical component of overdose risk reduction.
CDC Recommendations:
- Use the lowest effective dose and immediate-release formulations
- Avoid concurrent prescribing of opioids and benzodiazepines
- Reassess benefits and harms frequently, especially within 1–4 weeks of initiation
- Employ non-opioid therapies when feasible
Risk Stratification Tools
Clinicians should assess overdose risk before initiating opioid therapy:
- Opioid Risk Tool (ORT)
- Screener and Opioid Assessment for Patients with Pain (SOAPP)
- Prescription Drug Monitoring Programs (PDMPs) to monitor polypharmacy or doctor shopping
Naloxone Access and Distribution: A Lifesaving Strategy
Expanding Naloxone Availability
Naloxone, an opioid antagonist, reverses the effects of respiratory depression caused by overdose. Broad distribution is essential.
Community-Based Programs
- Standing orders for pharmacies to dispense naloxone without prescription
- Take-home naloxone kits for individuals using opioids or those at risk
- Training in overdose recognition and naloxone administration
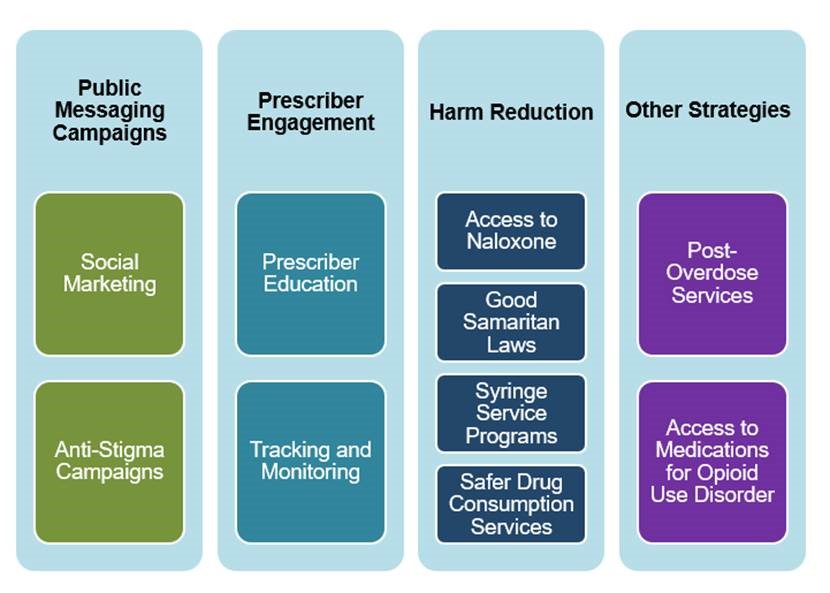
Harm Reduction Approaches for Overdose Prevention
Supervised Consumption Sites
Also known as Overdose Prevention Centers (OPCs), these facilities allow supervised use of opioids with immediate access to medical care, reducing overdose deaths and disease transmission.
Needle and Syringe Programs (NSPs)
These programs reduce the risks of HIV and hepatitis C among people who inject drugs, while also serving as access points for treatment referral and overdose education.
Education and Community Outreach
Public Awareness Campaigns
Dissemination of overdose prevention information helps destigmatize opioid use disorder and encourages help-seeking behavior. Campaigns should address:
- Safe storage and disposal of prescription opioids
- Recognition of overdose symptoms
- Importance of seeking emergency help
School and Workplace Programs
Targeted programs can educate youth and employees about opioid misuse risks and available resources, creating a culture of safety and awareness.
Integrating Substance Use Treatment with Risk Reduction
Medication-Assisted Treatment (MAT)
MAT using buprenorphine, methadone, or naltrexone reduces opioid cravings and the likelihood of fatal overdose. It should be:
- Widely accessible through primary care, specialized clinics, and correctional settings
- Combined with behavioral counseling
- Supported by insurance coverage and stigma reduction efforts
Continuity of Care After Nonfatal Overdose
Post-overdose care is a critical opportunity to initiate treatment:
- Emergency departments must offer brief interventions and referral
- Bridge programs provide rapid MAT initiation prior to long-term care placement
Policy and Legislative Measures
Prescription Monitoring Programs (PMPs)
Mandatory use of PMPs by prescribers helps identify high-risk prescribing patterns and prevents doctor shopping.
Good Samaritan Laws
These laws provide legal immunity to individuals who seek medical help during an overdose, encouraging bystanders to act without fear of prosecution.
Decriminalization and Diversion Programs
Shifting the approach from punitive to therapeutic allows individuals with opioid use disorder to receive treatment rather than incarceration, reducing recidivism and mortality.
Monitoring and Evaluation of Risk Mitigation Strategies
Evaluating the effectiveness of implemented measures is vital for sustained progress:
- Metrics include: Overdose mortality rates, naloxone distribution coverage, opioid prescribing trends, and treatment access
- Data sources: EMS reports, hospital admissions, prescription databases, and public health surveillance
Mitigating the risk of opioid overdose requires a multidimensional strategy rooted in clinical vigilance, harm reduction, and community engagement. With the integration of education, naloxone distribution, safe prescribing, and access to treatment, we can substantially reduce the burden of opioid overdose and save countless lives.