Rhinocerebral phycomycosis, also referred to as rhinocerebral mucormycosis, is a fulminant, angioinvasive fungal infection predominantly caused by fungi of the order Mucorales, especially Rhizopus species. This rare but rapidly progressing condition primarily affects immunocompromised individuals, particularly those with uncontrolled diabetes mellitus, especially in the context of ketoacidosis. Prompt diagnosis and aggressive management are critical to improve survival outcomes.
Etiology and Risk Factors
Causative Organisms
Phycomycosis is caused by saprophytic fungi from the class Zygomycetes, including:
- Rhizopus oryzae (most common)
- Mucor spp.
- Lichtheimia spp.
- Rhizomucor spp.
These organisms are ubiquitous in the environment and gain entry through inhalation of spores.
Predisposing Risk Factors
- Uncontrolled Diabetes Mellitus with Ketoacidosis
- Hematologic Malignancies
- Organ Transplantation
- Neutropenia
- Iron Overload or Deferoxamine Therapy
- Prolonged Corticosteroid Use
- COVID-19-Associated Immunosuppression
Pathogenesis of Rhinocerebral Mucormycosis
Upon inhalation, fungal spores colonize the nasal passages and sinuses. In susceptible hosts, the spores germinate and invade the vascular endothelium, leading to thrombosis, tissue necrosis, and rapid dissemination to adjacent structures such as the orbit and brain.
Clinical Manifestations
Early Symptoms
- Nasal congestion or sinusitis
- Facial pain or swelling, especially around the eyes
- Headache
- Black necrotic eschar on nasal turbinates or palate
Advanced Presentation
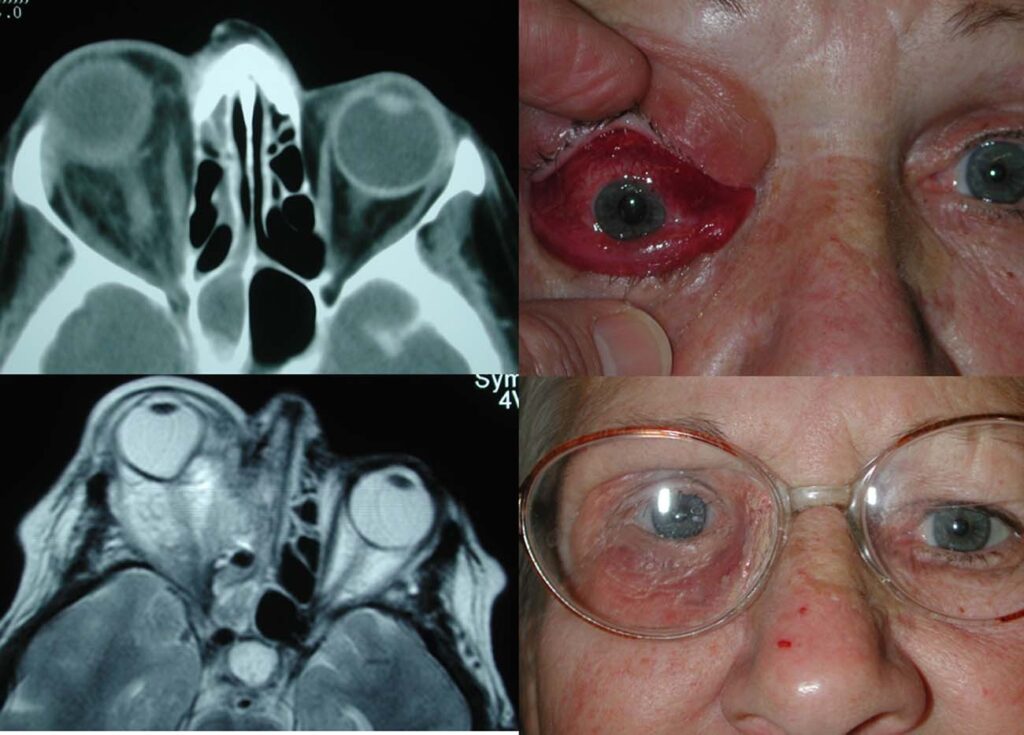
- Ophthalmoplegia
- Proptosis
- Vision loss
- Cranial nerve palsies (III, IV, V1/V2, VI)
- Altered mental status and seizures (indicating cerebral involvement)
- Fever and systemic signs of infection
Diagnostic Approach
Timely diagnosis of rhinocerebral phycomycosis is paramount due to its aggressive progression. Clinical suspicion in high-risk patients should prompt immediate evaluation.
Imaging Studies
- CT Scan of Paranasal Sinuses: Detects bone destruction, sinus opacification, and orbital extension
- MRI Brain and Orbit: Assesses soft tissue invasion and cerebral involvement
Microbiological Confirmation
- Direct KOH Mount of Nasal Tissue: Broad, ribbon-like, non-septate hyphae with right-angle branching
- Fungal Culture: Confirms species but is time-consuming
- Histopathological Examination: Demonstrates vascular invasion and necrosis
- PCR and Molecular Testing: Used in specialized settings
Differential Diagnosis
Rhinocerebral mucormycosis should be differentiated from:
- Bacterial Sinusitis
- Aspergillosis
- Granulomatosis with Polyangiitis
- Lymphoma or Other Neoplasms
- Tuberculosis of the Sinus
Management and Treatment Strategy
Treatment involves a multi-pronged approach requiring medical, surgical, and supportive care modalities.
1. Immediate Control of Underlying Risk Factors
- Rapid correction of diabetic ketoacidosis
- Cessation or reduction of immunosuppressive therapies
2. Antifungal Therapy
- First-line Drug: Liposomal Amphotericin B (5–10 mg/kg/day)
- Continue until clinical resolution and radiologic improvement
- Alternative/Adjunctive Agents:
- Posaconazole
- Isavuconazole
3. Aggressive Surgical Debridement
- Essential for removing necrotic tissue and reducing fungal burden
- May include:
- Endoscopic sinus surgery
- Orbital exenteration (in severe cases)
- Craniotomy for cerebral involvement
4. Adjunctive Therapies
- Hyperbaric Oxygen Therapy: Enhances neutrophil function and tissue oxygenation
- Iron Chelation (with agents other than deferoxamine): Experimental role
Prognosis and Mortality Rates
Despite treatment, rhinocerebral mucormycosis has high mortality, especially when diagnosis is delayed or when cerebral invasion occurs.
- Mortality Rates:
- Localized disease: ~30–50%
- Disseminated disease: >80%
Prognostic Factors:
- Early diagnosis and initiation of therapy
- Degree of immunosuppression
- Extent of surgical debridement
- Control of underlying conditions (e.g., diabetes)
Prevention and Surveillance in High-Risk Individuals
Risk Mitigation Strategies
- Tight glycemic control in diabetic patients
- Judicious use of corticosteroids and immunosuppressants
- Air filtration in hospital settings for immunocompromised patients
- Prophylactic antifungals in certain hematologic conditions (case-dependent)
Surveillance
- Regular ENT examinations in high-risk inpatients
- Early imaging when symptoms suggest sinus involvement
Case Insights and Epidemiological Considerations
Rising Incidence Post-COVID-19
A surge in mucormycosis cases, particularly in regions like India, was noted following the COVID-19 pandemic due to:
- Overuse of steroids
- Poor glycemic control
- Prolonged hospitalizations and mechanical ventilation
Rhinocerebral phycomycosis is a medical emergency demanding high clinical vigilance, especially in diabetic and immunocompromised patients. Early diagnosis, aggressive surgical and antifungal treatment, and management of underlying conditions are pivotal in improving survival. A multidisciplinary approach involving infectious disease specialists, otolaryngologists, ophthalmologists, and neurologists ensures optimal outcomes.