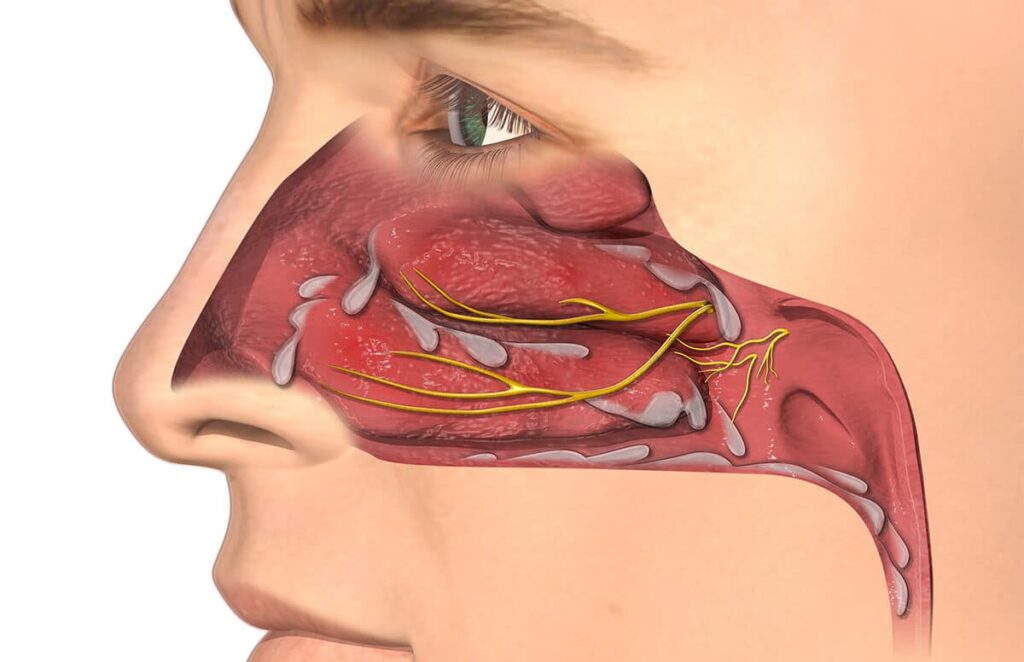
Rhinitis is the inflammation of the nasal mucosa, a condition characterized by symptoms such as nasal congestion, rhinorrhea (runny nose), sneezing, and itching. This widespread condition can be acute or chronic, allergic or non-allergic, and it significantly impacts quality of life and productivity. Prompt recognition and tailored management are essential for effective symptom control.
Classification of Rhinitis: Allergic vs. Non-Allergic Variants
Allergic Rhinitis (AR)
Allergic rhinitis is an IgE-mediated hypersensitivity response to environmental allergens such as pollen, dust mites, pet dander, or mold.
Types of Allergic Rhinitis:
- Seasonal Allergic Rhinitis (Hay Fever): Triggered by airborne pollens during specific times of the year.
- Perennial Allergic Rhinitis: Occurs year-round, usually due to indoor allergens.
Clinical Features:
- Nasal congestion
- Sneezing
- Itchy nose, eyes, or throat
- Postnasal drip
- Watery rhinorrhea
Non-Allergic Rhinitis (NAR)
Non-allergic rhinitis includes a range of conditions with similar symptoms but without an allergic basis.
Subtypes Include:
- Vasomotor Rhinitis: Triggered by irritants like smoke, odors, or temperature changes
- Infectious Rhinitis: Typically viral, associated with the common cold
- Hormonal Rhinitis: Seen in pregnancy or with thyroid disorders
- Drug-Induced Rhinitis: Caused by overuse of nasal decongestants (rhinitis medicamentosa)
- Gustatory Rhinitis: Induced by consumption of hot or spicy food
Etiology: Causes and Risk Factors
Rhinitis results from complex interactions between genetic and environmental factors.
Common Causes:
- Environmental Allergens
- Air Pollutants and Tobacco Smoke
- Viral Infections
- Occupational Irritants
- Hormonal Changes
- Certain Medications (e.g., NSAIDs, beta-blockers)
Risk Factors:
- Family history of allergies or asthma
- Living in urban environments
- Occupational exposure to irritants
- Nasal anatomical abnormalities (e.g., deviated septum)
Diagnosis of Rhinitis: Accurate Identification is Crucial
Clinical Evaluation
A thorough patient history and physical examination are fundamental.
Key Diagnostic Questions:
- Are symptoms seasonal or year-round?
- Is there an identifiable trigger?
- Are there coexisting conditions such as asthma or conjunctivitis?
Diagnostic Tests
- Skin Prick Testing: To identify specific allergens
- Serum Specific IgE Testing: Quantifies allergic sensitivity
- Nasal Endoscopy: Visualizes structural abnormalities or signs of chronic inflammation
- CT Scan of Sinuses: For patients with persistent or complicated rhinitis
- Nasal Cytology: Helps differentiate between allergic and non-allergic causes
Treatment Strategies for Rhinitis
Allergen Avoidance
The first line of defense for allergic rhinitis is the identification and avoidance of known allergens.
Examples:
- Use of HEPA filters
- Dust mite-proof bedding
- Minimizing outdoor activity during pollen seasons
- Removing mold or pet dander
Pharmacologic Therapy
1. Antihistamines:
Block histamine receptors to reduce sneezing and itching
- Examples: Cetirizine, Loratadine, Fexofenadine
2. Intranasal Corticosteroids:
Most effective for inflammation control
- Examples: Fluticasone, Mometasone, Budesonide
3. Decongestants:
Reduce nasal swelling but not for long-term use
- Examples: Pseudoephedrine, Oxymetazoline
4. Leukotriene Receptor Antagonists:
Useful in coexisting asthma
- Example: Montelukast
5. Anticholinergic Nasal Sprays:
Target rhinorrhea
- Example: Ipratropium bromide
6. Nasal Saline Irrigation:
Helpful for both allergic and non-allergic rhinitis
Immunotherapy (Allergy Shots)
A long-term solution for allergic rhinitis, especially when pharmacologic therapy is insufficient.
- Subcutaneous or sublingual options
- Alters immune response over time
Management of Non-Allergic Rhinitis
Treatment varies depending on subtype:
- Vasomotor Rhinitis: Avoid triggers, use nasal corticosteroids or anticholinergics
- Rhinitis Medicamentosa: Discontinue offending nasal spray, initiate corticosteroids
- Gustatory Rhinitis: Managed with anticholinergic sprays
- Hormonal Rhinitis: Supportive care, symptoms often resolve postpartum
Complications of Untreated Rhinitis
- Chronic Sinusitis
- Nasal Polyps
- Otitis Media (especially in children)
- Sleep Disorders including Obstructive Sleep Apnea
- Reduced Quality of Life and Work Productivity
Rhinitis in Special Populations
Pediatric Rhinitis
- Often underdiagnosed
- Needs careful differentiation between viral and allergic causes
- Nasal corticosteroids are safe and effective when used appropriately
Geriatric Patients
- More likely to suffer from non-allergic rhinitis
- Increased risk of medication side effects
- Consideration of polypharmacy essential
Preventive Measures and Lifestyle Modifications
- Maintain indoor air quality
- Use allergen-proof home fixtures
- Keep pets out of bedrooms
- Avoid smoking and passive smoke exposure
- Engage in regular nasal hygiene with saline rinses
Rhinitis, whether allergic or non-allergic, demands a nuanced diagnostic and therapeutic approach tailored to the individual. Proper classification, thorough evaluation, and comprehensive treatment are essential to achieve optimal symptom control and prevent long-term complications. By implementing both pharmacologic and non-pharmacologic strategies, we can significantly enhance patient outcomes and quality of life.