Treating rheumatoid arthritis (RA) in patients with an elevated risk of gastric ulcers presents a significant clinical challenge. These patients require anti-inflammatory therapy to control autoimmune joint inflammation while minimizing the gastrointestinal (GI) complications frequently associated with conventional treatment options. Effective management requires a tailored approach that balances disease control with gastroprotection.
Pathophysiology of RA and Its Implications for GI Risk
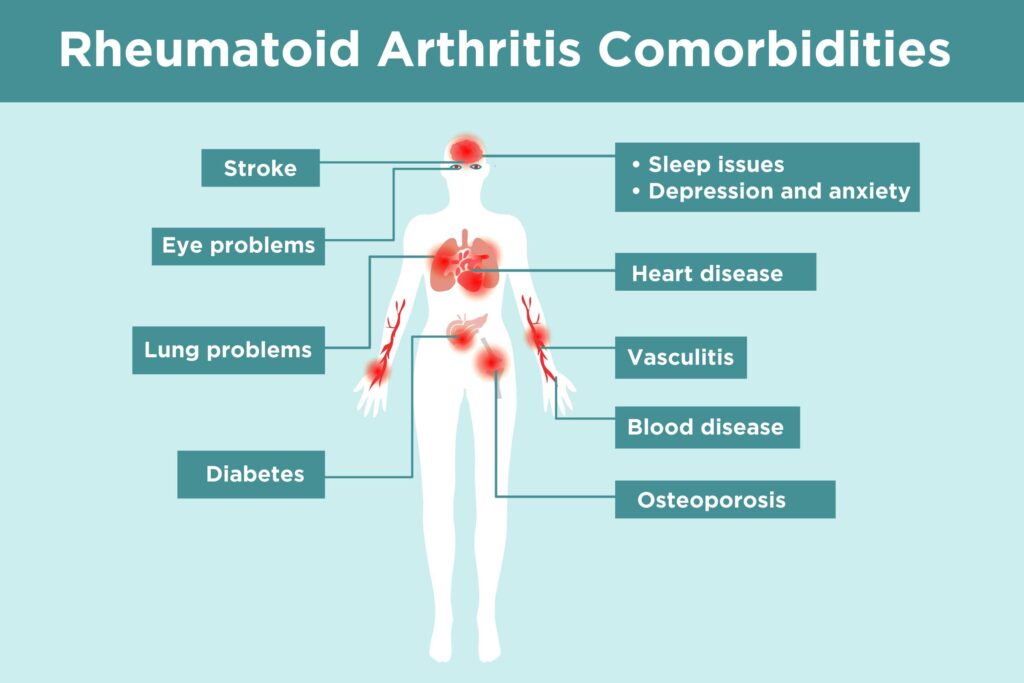
Rheumatoid arthritis is a systemic autoimmune disorder marked by chronic synovial inflammation, leading to joint destruction and disability. First-line treatment typically includes nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids—both of which are known contributors to gastrointestinal mucosal injury.
Patients at high gastric ulcer risk may include:
- Individuals aged ≥65 years
- History of peptic ulcer disease or GI bleeding
- Concurrent use of corticosteroids or anticoagulants
- Helicobacter pylori infection
- High-dose or long-term NSAID users
Risk Stratification and Preventive Strategies
Identifying High-Risk RA Patients
Risk stratification is crucial in guiding therapeutic choices. We assess the following:
- Prior upper GI events
- Current or planned NSAID use
- Comorbidities (e.g., cardiovascular disease, renal impairment)
- Concomitant medications (e.g., aspirin, SSRIs, corticosteroids)
Protective Measures
- Eradication of H. pylori when detected
- Use of gastroprotective agents, including proton pump inhibitors (PPIs)
- Avoidance of nonselective NSAIDs unless necessary
- Consideration of COX-2 selective inhibitors, which offer reduced GI toxicity
Pharmacologic Approaches in High Ulcer-Risk Patients
1. Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs remain the cornerstone of RA therapy and are preferred in high-GI-risk populations due to their disease-targeting mechanism and minimal GI side effects.
Common Conventional DMARDs:
- Methotrexate
- Leflunomide
- Sulfasalazine
- Hydroxychloroquine
These agents should be initiated early and monitored for hepatic, hematologic, and pulmonary adverse effects, but they are not major contributors to gastric ulcer risk.
2. Biologic DMARDs and Targeted Synthetic DMARDs
Biologic therapies and JAK inhibitors offer effective inflammation control without direct GI mucosal toxicity.
- TNF-α inhibitors: Etanercept, Infliximab
- IL-6 receptor antagonists: Tocilizumab
- JAK inhibitors: Tofacitinib, Baricitinib
These are typically used in patients with inadequate response to conventional DMARDs.
3. NSAID Use: Balancing Pain Relief with Gastric Safety
NSAIDs, while effective for symptom relief, carry high GI risks. When their use is unavoidable:
- Prefer COX-2 inhibitors (e.g., Celecoxib)
- Co-prescribe PPIs for ulcer prophylaxis
- Use lowest effective dose for shortest duration
- Consider non-NSAID analgesics (e.g., acetaminophen, tramadol)
Gastroprotective Strategies
Proton Pump Inhibitors (PPIs)
PPIs such as omeprazole, esomeprazole, and pantoprazole are the first-line agents for preventing NSAID-induced ulcers and bleeding. They reduce gastric acid secretion, facilitating mucosal healing.
H2-Receptor Antagonists
Less effective than PPIs for ulcer prevention, but may be considered when PPI use is contraindicated.
Misoprostol
A prostaglandin analog that offers mucosal protection but may cause diarrhea and abdominal cramping.
Monitoring and Follow-Up
Routine follow-up is essential to ensure disease control while avoiding gastrointestinal complications.
Regular Assessments Include:
- Disease Activity Score (DAS28)
- GI symptom review
- Laboratory monitoring (CBC, LFTs, renal function)
- Endoscopic surveillance in patients with persistent GI symptoms or bleeding risk
Patient Education and Lifestyle Measures
Empowering patients with knowledge about their medications and potential side effects significantly enhances treatment adherence and outcomes.
Key Counseling Points:
- Recognize early signs of GI bleeding (e.g., black stools, abdominal pain)
- Avoid alcohol and smoking
- Maintain a diet that supports GI health
- Adhere to medication regimens precisely
In patients with rheumatoid arthritis and high gastric ulcer risk, the therapeutic strategy must minimize gastrointestinal complications without compromising disease control. This requires prioritizing DMARDs, judicious use of NSAIDs, and the integration of gastroprotective agents. With a personalized and evidence-based approach, we can effectively manage RA while safeguarding against ulcer-related morbidity.