Rheumatic fever is an autoimmune inflammatory disease that can develop after an untreated or inadequately treated Group A streptococcal (GAS) pharyngitis, commonly known as strep throat. It primarily affects children aged 5 to 15 years and is a leading cause of acquired heart disease in young individuals worldwide. Rheumatic fever is most prevalent in low- and middle-income countries with limited access to healthcare and streptococcal diagnostics.
Pathophysiology and Immune Response
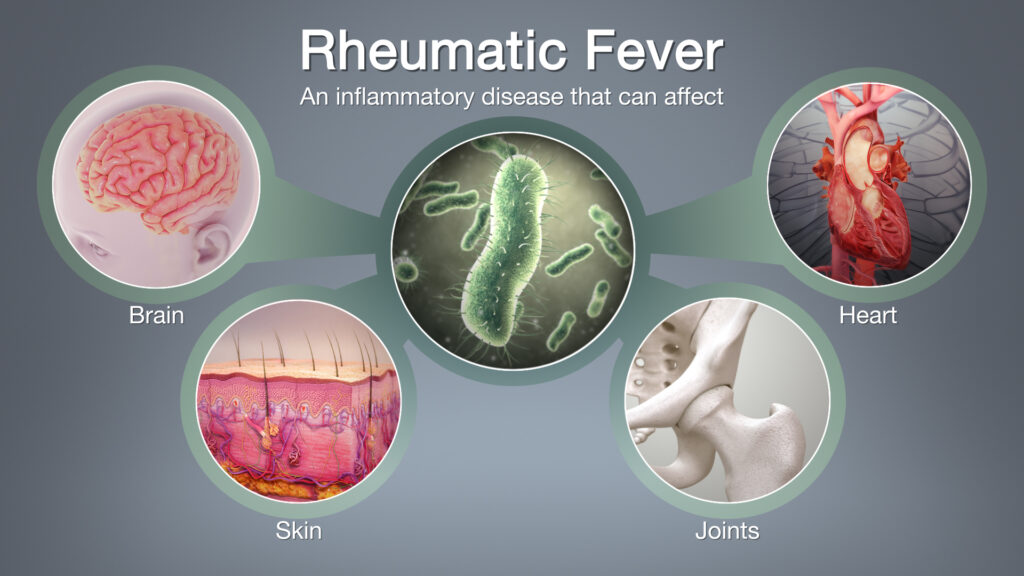
Rheumatic fever is triggered by an aberrant immune reaction following streptococcal infection. The body produces antibodies targeting the M protein of Streptococcus pyogenes, which cross-react with host tissues in the heart, joints, skin, and central nervous system. This molecular mimicry leads to widespread inflammation and tissue damage, particularly in the cardiac valves.
Clinical Features of Rheumatic Fever
The clinical manifestations vary depending on the organs involved and typically appear 2 to 4 weeks after a GAS throat infection.
Major Manifestations (per Jones Criteria)
- Carditis: May involve endocardium, myocardium, and pericardium. Can lead to mitral or aortic regurgitation.
- Polyarthritis: Migratory, affecting large joints (knees, ankles, elbows).
- Sydenham Chorea: Involuntary, rapid movements of face and limbs; often appears later.
- Erythema Marginatum: Non-pruritic, serpiginous rash typically on trunk.
- Subcutaneous Nodules: Firm, painless nodules over bony prominences.
Minor Criteria
- Fever
- Arthralgia
- Elevated acute-phase reactants (ESR, CRP)
- Prolonged PR interval on ECG
A confirmed diagnosis typically requires evidence of a preceding streptococcal infection and either:
- Two major criteria, or
- One major and two minor criteria.
Diagnostic Evaluation
Timely diagnosis is critical to prevent irreversible cardiac damage. Diagnosis is primarily clinical, supported by laboratory and imaging studies:
- Throat Culture or Rapid Antigen Test: Confirms recent streptococcal infection.
- Anti-streptolysin O (ASO) Titers: Elevated levels indicate recent GAS exposure.
- Echocardiogram: Detects valvular involvement and cardiac function.
- Electrocardiogram (ECG): May show PR interval prolongation.
- Blood Tests: Elevated ESR, CRP, and leukocytosis support inflammation.
Treatment and Management
Acute Phase Management
- Antibiotics: Penicillin (oral or intramuscular) to eradicate streptococcal bacteria.
- Anti-inflammatory Therapy: Aspirin or corticosteroids to reduce joint and cardiac inflammation.
- Bed Rest: Recommended during acute carditis.
- Anticonvulsants or Sedatives: For patients with Sydenham chorea.
Long-Term Prophylaxis
To prevent recurrence and further cardiac damage, patients receive long-term antibiotic prophylaxis:
- Intramuscular Benzathine Penicillin G: Every 3 to 4 weeks.
- Duration: Typically 5 years or until age 21 for those without carditis; up to 10 years or more for patients with carditis.
Complications of Rheumatic Fever
The most serious long-term consequence is rheumatic heart disease (RHD), resulting from repeated inflammation and scarring of the heart valves. Other complications include:
- Chronic valvular stenosis or regurgitation
- Congestive heart failure
- Atrial fibrillation
- Infective endocarditis
Early detection and secondary prophylaxis are key to reducing RHD burden.
Prevention Strategies
Primary Prevention
- Prompt diagnosis and treatment of strep throat with antibiotics (especially in high-risk populations).
- Health education to promote early medical consultation for sore throats.
Secondary Prevention
- Long-term antibiotic prophylaxis in individuals with a history of rheumatic fever.
- Regular follow-up and echocardiography for monitoring cardiac function.
Prognosis and Global Burden
With appropriate treatment, the prognosis of rheumatic fever is generally good, especially in cases without carditis. However, in regions lacking access to healthcare, delayed diagnosis and inadequate prophylaxis contribute to a higher incidence of RHD and related mortality.
The global burden remains significant, with millions affected and an estimated 275,000 deaths annually due to complications of rheumatic heart disease.
Rheumatic fever remains a major public health issue, particularly in underserved regions. Effective control requires early recognition, prompt antibiotic therapy, and consistent long-term prophylaxis. Continued awareness, improved healthcare access, and global public health initiatives are essential to mitigate the long-term complications of this preventable disease.

