Renal disease with edema refers to kidney conditions where the body retains excess fluid, leading to swelling or edema, particularly in the legs, ankles, and around the eyes. This swelling occurs when the kidneys are unable to properly filter and remove waste, salt, and excess fluids from the body. Edema associated with renal disease can be a sign of severe kidney dysfunction or an underlying health issue, and understanding the causes and management of this condition is crucial for those affected.
What is Renal Disease with Edema?
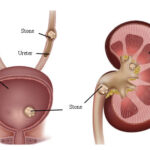
Renal disease with edema is typically characterized by the inability of the kidneys to maintain the body’s fluid and electrolyte balance. When the kidneys are damaged or compromised, they may not function properly, causing the body to retain water. The excess fluid accumulates in the tissues, resulting in swelling (edema). This condition can affect various parts of the body, but it is most commonly observed in the lower extremities. In some cases, edema can also occur in the abdomen or lungs.
Causes of Edema in Renal Disease
Edema in renal disease is primarily caused by the kidneys’ inability to excrete excess sodium and water. Several underlying conditions can lead to this problem, including:
- Chronic Kidney Disease (CKD): As kidney function declines, the kidneys lose their ability to filter waste and excess fluid effectively, leading to fluid buildup and edema.
- Nephrotic Syndrome: This condition results from damage to the glomeruli (the filtering units of the kidneys), leading to protein loss in the urine and a decrease in the blood protein albumin, which helps maintain fluid balance.
- Acute Kidney Injury (AKI): Sudden kidney dysfunction caused by injury or illness can lead to fluid retention and edema, often accompanied by other symptoms such as decreased urine output.
- Heart Failure: While primarily a cardiac condition, heart failure can cause kidney dysfunction due to reduced blood flow, contributing to edema and renal complications.
- Liver Disease (Cirrhosis): Liver diseases like cirrhosis can also affect kidney function, leading to fluid retention and edema, especially in the abdomen (ascites).
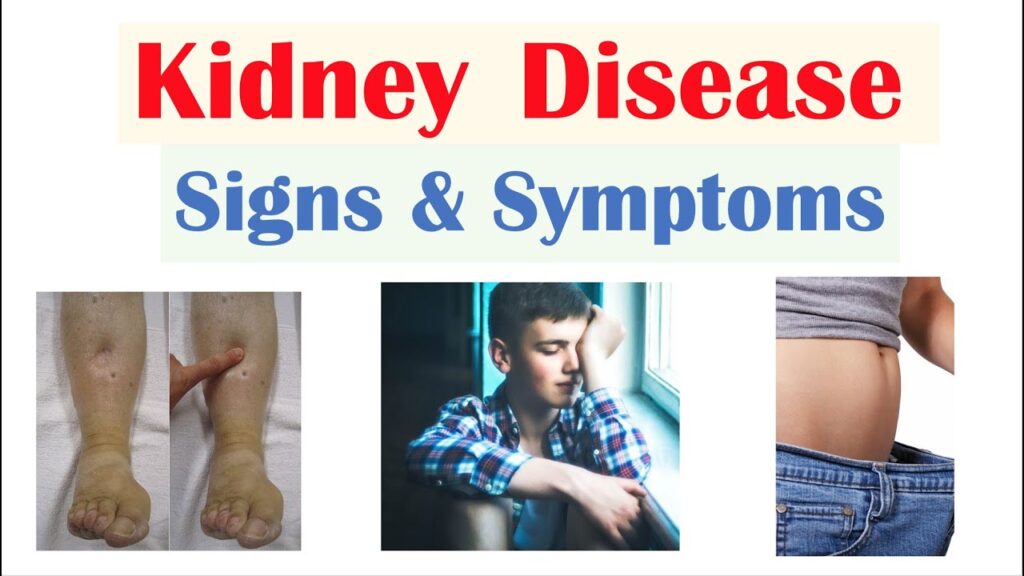
Symptoms of Renal Disease with Edema
The primary symptom of renal disease with edema is swelling, but other signs may also be present. These include:
- Swelling in the Legs, Ankles, and Feet: This is the most common area where edema is noticeable, particularly after standing or walking for extended periods.
- Swelling around the Eyes: Particularly in the morning, swelling around the eyes can indicate protein loss through the kidneys and impaired fluid regulation.
- Shortness of Breath: If fluid accumulates in the lungs, it can cause shortness of breath, a serious complication known as pulmonary edema.
- Fatigue and Weakness: Due to the buildup of waste products in the body and the body’s struggle to regulate fluids and electrolytes, people with renal disease and edema often experience fatigue and general weakness.
- Reduced Urine Output: A decrease in urine production can occur due to kidney dysfunction, contributing to fluid retention.
Diagnosing Renal Disease with Edema
Diagnosing renal disease with edema typically involves a combination of clinical evaluation and diagnostic tests. Key diagnostic tools include:
- Urinalysis: This test checks for protein in the urine, which is a hallmark sign of nephrotic syndrome and other renal diseases that lead to edema.
- Blood Tests: Blood tests measure kidney function by assessing levels of creatinine, blood urea nitrogen (BUN), and electrolytes. Elevated levels of these substances can indicate kidney dysfunction.
- Ultrasound: Kidney ultrasound can help evaluate kidney size and structure, checking for signs of damage or disease.
- CT Scan or MRI: In some cases, more detailed imaging may be required to evaluate the kidneys and identify any underlying structural problems.
- Kidney Biopsy: In certain situations, a biopsy may be necessary to obtain a tissue sample from the kidneys for further examination, particularly when the cause of the kidney disease is unclear.
Treatment of Renal Disease with Edema
The treatment of renal disease with edema focuses on both managing the underlying condition and reducing fluid retention. Key treatment strategies include:
1. Managing the Underlying Kidney Disease
Treatment begins with addressing the root cause of kidney dysfunction. This may involve:
- Medication for Kidney Disease: Angiotensin-converting enzyme inhibitors (ACE inhibitors) and angiotensin receptor blockers (ARBs) are commonly prescribed to manage kidney disease, particularly in CKD.
- Immunosuppressive Therapy: For conditions like nephrotic syndrome, medications to suppress the immune system and reduce kidney inflammation may be necessary.
- Dialysis: In advanced cases of kidney failure, dialysis may be required to remove excess fluid and waste products from the body.
2. Fluid and Sodium Management
Patients with renal disease and edema often need to manage fluid and sodium intake carefully. Recommendations may include:
- Limiting Sodium Intake: Reducing sodium intake helps prevent fluid retention and alleviate edema symptoms.
- Diuretics: Diuretic medications help the body expel excess fluid by increasing urine production. They are commonly used in patients with heart failure and kidney disease to control edema.
3. Lifestyle Changes
Certain lifestyle modifications can help improve kidney function and reduce fluid retention, including:
- Regular Exercise: Engaging in moderate physical activity can help improve circulation and reduce swelling.
- Dietary Modifications: A low-sodium, low-potassium, and balanced diet can support kidney health and fluid balance.
- Weight Management: Maintaining a healthy weight reduces the strain on the kidneys and can help prevent the progression of renal disease.
Preventing Edema in Renal Disease
Prevention of edema in renal disease largely revolves around early detection and proper management of kidney function. Key strategies include:
- Routine Kidney Function Monitoring: Regular blood and urine tests can help detect early signs of kidney disease, enabling prompt intervention.
- Managing Underlying Conditions: Controlling high blood pressure, diabetes, and other comorbidities can reduce the risk of kidney damage and fluid retention.
- Adhering to Treatment Plans: Following prescribed medications, dietary recommendations, and lifestyle changes can help prevent edema and kidney disease progression.
Complications of Renal Disease with Edema
If left untreated, renal disease with edema can lead to serious complications, including:
- Pulmonary Edema: Fluid buildup in the lungs can cause breathing difficulties and may be life-threatening if not managed promptly.
- Electrolyte Imbalance: Fluid retention and kidney dysfunction can lead to dangerous electrolyte imbalances, affecting heart and muscle function.
- Kidney Failure: Advanced kidney disease can lead to complete kidney failure, necessitating dialysis or a kidney transplant.
Renal disease with edema is a serious condition that requires timely diagnosis and effective management. By understanding the causes, symptoms, diagnosis, and treatment options, individuals with kidney disease can take proactive steps to manage their condition and prevent further complications. Early intervention, proper treatment, and lifestyle modifications play a vital role in controlling fluid retention and preserving kidney function.