Renal cell carcinoma (RCC) is the most prevalent form of kidney cancer, originating in the cells of the renal tubules. A nephrectomy, which is the surgical removal of a kidney, is often the primary treatment for RCC, especially when the cancer is localized. However, for many patients, additional therapies are required after nephrectomy to reduce the risk of recurrence and improve overall survival. This is where adjuvant therapy plays a crucial role in the management of RCC following nephrectomy.
Adjuvant therapy refers to treatments given after the primary surgery to eliminate any remaining cancer cells, reduce the risk of recurrence, and improve patient outcomes. This article provides a detailed exploration of the role of adjuvant therapy in RCC following nephrectomy, the available options, their effectiveness, and the latest developments in this area.
What is Adjuvant Therapy?
Adjuvant therapy is designed to complement the primary treatment—in this case, nephrectomy. While nephrectomy is effective in removing the tumor from the kidney, microscopic cancer cells may remain in the body, potentially leading to recurrence. Adjuvant therapies are used after surgery to target these remaining cells and reduce the risk of relapse.
Types of Adjuvant Therapy in RCC
Several types of adjuvant therapies are considered for use in RCC, including immunotherapy, targeted therapy, and radiation therapy. The choice of therapy depends on factors such as the stage of cancer, the patient’s overall health, and the characteristics of the tumor.
Adjuvant Immunotherapy in RCC
Immunotherapy has emerged as a critical component of RCC treatment, especially after nephrectomy. This treatment works by stimulating the patient’s immune system to recognize and attack cancer cells. Immunotherapy can be used in patients with high-risk RCC to prevent recurrence.
Immune Checkpoint Inhibitors
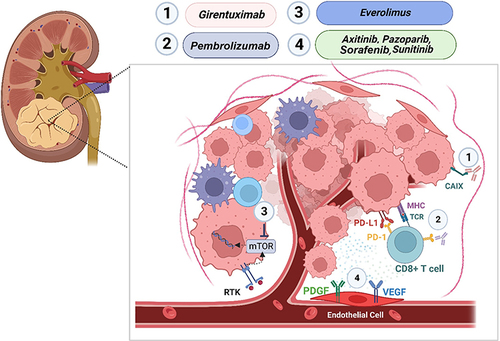
Immune checkpoint inhibitors, such as nivolumab and pembrolizumab, have shown promise in the adjuvant setting following nephrectomy. These drugs work by blocking proteins that inhibit the immune system’s ability to detect and attack cancer cells. In RCC, nivolumab has been approved for use as an adjuvant therapy following nephrectomy in high-risk patients, particularly those with stage II or higher disease.
The CheckMate 914 trial, which evaluated the efficacy of nivolumab in the adjuvant setting, demonstrated that nivolumab significantly reduced the risk of recurrence in patients with intermediate- or high-risk RCC, highlighting the potential of this therapy to improve outcomes after surgery.
Cytokine Therapy
Cytokine therapy, specifically interleukin-2 (IL-2), has historically been used in the treatment of RCC. Although it is less commonly used today due to its toxicity and side effects, IL-2 remains an option for certain high-risk patients, particularly those with metastatic disease or those undergoing aggressive treatment plans.
Targeted Therapy in RCC
Targeted therapy uses drugs that specifically target molecular pathways involved in cancer cell growth and survival. These therapies are increasingly used in the adjuvant setting following nephrectomy to reduce the risk of RCC recurrence.
Tyrosine Kinase Inhibitors (TKIs)
Tyrosine kinase inhibitors (TKIs) are one of the most widely used forms of targeted therapy for RCC. These drugs target specific enzymes involved in tumor growth, such as sunitinib, pazopanib, and axitinib. While TKIs are primarily used in metastatic RCC, they have also been studied for use in the adjuvant setting.
In the S-TRAC trial, sunitinib was shown to improve disease-free survival in high-risk patients following nephrectomy. Although the benefits of TKIs in the adjuvant setting are still being evaluated, they remain an important consideration for patients with high-risk RCC after surgery.
mTOR Inhibitors
Everolimus, an mTOR inhibitor, is another targeted therapy that has been explored in the adjuvant setting for RCC. This drug works by inhibiting the mTOR pathway, which is involved in cell growth and division. While everolimus is typically used in metastatic RCC, it has shown promise in reducing recurrence after nephrectomy, particularly in patients with certain genetic mutations or high-risk disease.
Radiation Therapy in RCC
Although not commonly used in RCC, radiation therapy may be employed in select cases after nephrectomy. This is typically reserved for patients with locally advanced RCC or those with metastasis to other organs, such as the lungs or bones.
Role of Radiation Therapy in the Adjuvant Setting
Postoperative radiation therapy may be considered in patients who have undergone a nephrectomy but still have a high risk of recurrence. Radiation is primarily used to target small tumor remnants or to alleviate symptoms related to metastasis. However, its use in RCC is limited, and its benefits in the adjuvant setting are still debated.
Prognostic Factors and Risk Stratification
The decision to administer adjuvant therapy following nephrectomy depends on several factors that assess the risk of recurrence and the potential benefit of additional treatment. These include:
- Stage of the Cancer: The more advanced the stage of RCC, the higher the risk of recurrence. High-risk patients, such as those with stage II or higher disease, may benefit from adjuvant therapy.
- Histological Features: Tumors with aggressive histological features, such as high-grade tumors or those with sarcomatoid differentiation, are associated with a higher likelihood of recurrence and may warrant adjuvant treatment.
- Molecular Markers: Emerging research into molecular markers, such as PD-L1 expression and mutations in the VHL gene, may help identify patients who are more likely to benefit from adjuvant therapy.
Current Guidelines and Recommendations
The management of RCC after nephrectomy is evolving, with several major guidelines offering recommendations for adjuvant therapy.
- National Comprehensive Cancer Network (NCCN): The NCCN recommends considering adjuvant immunotherapy for high-risk patients following nephrectomy, especially those with stage II or higher RCC. Immune checkpoint inhibitors such as nivolumab are recommended for these patients.
- European Association of Urology (EAU): The EAU also recognizes the potential of adjuvant immunotherapy and targeted therapy, but stresses the importance of patient-specific risk factors in deciding on adjuvant treatment.
Challenges and Future Directions
While adjuvant therapies have shown promise in improving outcomes for RCC patients after nephrectomy, several challenges remain. These include the identification of the most effective therapies for individual patients, managing side effects, and determining the optimal duration of treatment. Ongoing clinical trials and research into the molecular biology of RCC are expected to provide more insights into these areas and help refine treatment approaches in the future.
Clinical Trials and Emerging Therapies
Several clinical trials are currently underway to evaluate new adjuvant therapies for RCC. These include combinations of immunotherapy and targeted therapies, as well as new drugs targeting different molecular pathways involved in RCC. The results of these trials may provide new opportunities for more effective and personalized adjuvant treatment strategies in the coming years.
Adjuvant therapy following nephrectomy plays a critical role in the management of renal cell carcinoma, particularly in high-risk patients. While immunotherapy and targeted therapy have demonstrated significant promise, further research is needed to determine the most effective approaches for different patient populations. With advances in molecular medicine and personalized oncology, the future of adjuvant therapy for RCC appears promising, offering hope for improved survival and reduced recurrence for patients worldwide.