Relapsing-Remitting Multiple Sclerosis (RRMS) is the most common form of multiple sclerosis (MS), a chronic autoimmune disease that affects the central nervous system (CNS). MS occurs when the body’s immune system mistakenly attacks the protective covering of nerve fibers, known as myelin, causing inflammation and damage. In RRMS, individuals experience episodes of neurological decline (relapses) followed by periods of recovery (remission), with symptoms improving or even disappearing between relapses.
Understanding the intricacies of RRMS, including its causes, symptoms, diagnostic methods, and treatment options, is crucial for patients, caregivers, and healthcare professionals. This comprehensive guide aims to provide all the essential information needed to navigate the complexities of RRMS, manage the disease, and improve the quality of life for those affected.
What is Relapsing-Remitting Multiple Sclerosis?
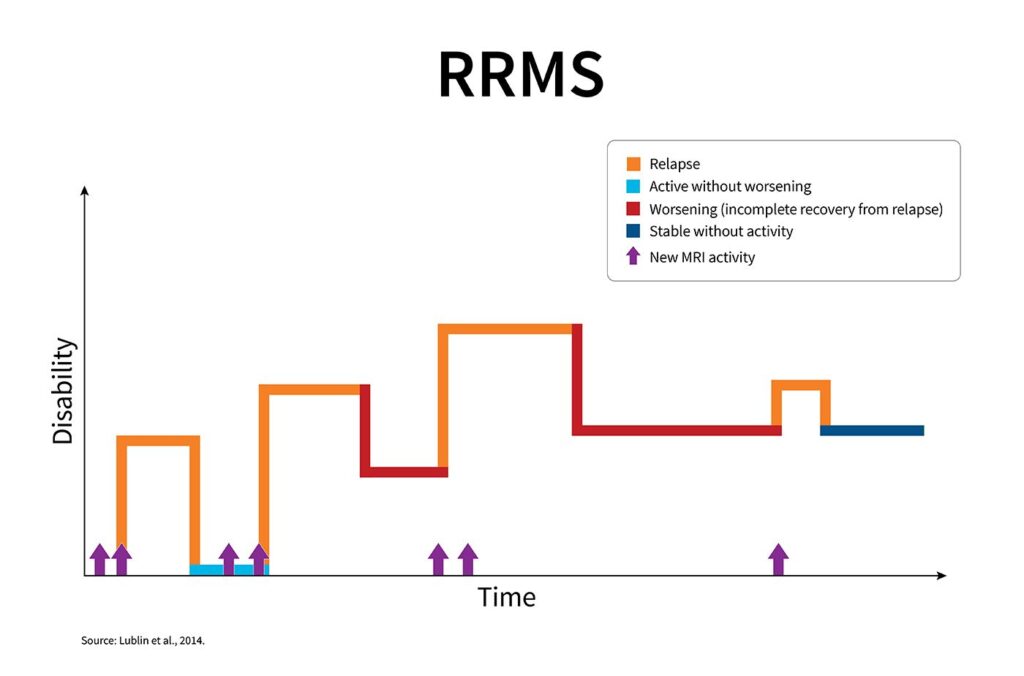
Relapsing-Remitting Multiple Sclerosis is characterized by distinct phases of exacerbation and recovery. During a relapse, new or worsening symptoms emerge, often due to inflammation and damage to myelin in the CNS. Following the relapse, patients typically experience a period of remission, where symptoms improve or stabilize.
Although RRMS is considered to be the most manageable form of MS, it can evolve into secondary progressive multiple sclerosis (SPMS) over time, where symptoms gradually worsen without the distinct periods of relapse and remission. Early intervention and proper management can help slow this progression.
Key Features of RRMS
- Relapses: New or worsening neurological symptoms that typically last for at least 24 hours, often triggered by immune system attacks on the myelin.
- Remission: A period where symptoms improve or completely disappear, allowing the individual to regain lost functions.
- No Permanent Disability: Unlike progressive forms of MS, RRMS patients may not experience constant disability, although the risk of progression remains.
Causes and Risk Factors of RRMS
The exact cause of relapsing-remitting multiple sclerosis remains unclear, but it is generally believed to involve a combination of genetic and environmental factors that trigger an autoimmune response against the CNS.
Genetic Factors
Certain genes, especially those associated with the immune system, may predispose individuals to MS. While having a family history of MS increases the risk, the condition is not directly inherited.
Environmental Triggers
- Vitamin D Deficiency: Low levels of vitamin D have been associated with a higher risk of developing MS. Exposure to sunlight, which helps the body produce vitamin D, may play a role in reducing the risk.
- Geographic Location: MS is more prevalent in countries farther from the equator, suggesting that environmental factors such as sunlight exposure and vitamin D levels may influence the risk of developing MS.
- Infections: Certain viral infections, such as Epstein-Barr virus (EBV), have been linked to an increased risk of MS, though the exact mechanism remains under investigation.
Gender and Age
RRMS is more common in women than in men, with a ratio of approximately 3:1. The disease typically begins in young adulthood, between the ages of 20 and 40. However, it can develop at any age.
Symptoms of Relapsing-Remitting Multiple Sclerosis
Symptoms of RRMS vary significantly from person to person and can affect different parts of the CNS. Symptoms may appear suddenly during a relapse and can include:
Neurological Symptoms
- Numbness or Tingling: A common symptom affecting the limbs or face, often accompanied by a sensation of “pins and needles.”
- Muscle Weakness: Weakness in the arms or legs may occur, affecting mobility and coordination.
- Vision Problems: Inflammation of the optic nerve (optic neuritis) can cause blurred vision, double vision, or even temporary vision loss in one eye.
- Balance and Coordination Issues: Difficulty maintaining balance, dizziness, or clumsiness is common during relapses.
- Fatigue: One of the most disabling symptoms, fatigue in MS is often disproportionate to activity levels and can significantly affect daily functioning.
Cognitive and Emotional Symptoms
- Cognitive Dysfunction: Memory problems, difficulty concentrating, and reduced processing speed may occur, especially during periods of relapse.
- Mood Changes: Depression, anxiety, and mood swings are common in RRMS, often exacerbated by the challenges of living with a chronic condition.
Bowel and Bladder Dysfunction
- Bladder Issues: MS can affect the nerves controlling bladder function, leading to urinary urgency, frequency, or incontinence.
- Bowel Dysfunction: Constipation or difficulty with bowel control can occur, often linked to muscle weakness or nerve damage.
Diagnosing Relapsing-Remitting Multiple Sclerosis
Diagnosing RRMS involves a combination of clinical evaluation, medical history, imaging tests, and laboratory studies. The diagnostic process typically includes the following steps:
Clinical Evaluation
A neurologist will assess the patient’s symptoms, medical history, and any past episodes of neurological issues. A thorough examination of reflexes, muscle strength, coordination, and sensory function is performed.
Magnetic Resonance Imaging (MRI)
MRI is the most common imaging technique used to diagnose MS. It helps detect areas of demyelination, known as lesions, in the brain and spinal cord. MRI can show both active lesions (indicating ongoing inflammation) and older, inactive lesions.
Lumbar Puncture (Spinal Tap)
A lumbar puncture may be performed to analyze cerebrospinal fluid (CSF) for the presence of abnormal proteins or immune cells associated with MS. This test can help confirm the diagnosis when combined with other findings.
Evoked Potentials
Evoked potentials measure the electrical activity in the brain in response to visual, auditory, or sensory stimuli. This test can help identify nerve damage in areas that may not be easily detectable by other methods.
Treatment Options for Relapsing-Remitting Multiple Sclerosis
While there is no cure for RRMS, there are several treatment options that can help manage symptoms, reduce relapses, and slow the progression of the disease. Treatment strategies typically involve medications, lifestyle modifications, and symptom management.
Disease-Modifying Therapies (DMTs)
DMTs are the cornerstone of MS treatment. These medications are designed to reduce the frequency and severity of relapses, slow the accumulation of disability, and decrease the number of new lesions in the CNS. Common DMTs for RRMS include:
- Interferon Beta: An immune-modulating drug that reduces inflammation and immune cell activity.
- Glatiramer Acetate: Another immune-modulating drug that helps prevent attacks on the myelin.
- Oral Medications: Drugs like fingolimod and dimethyl fumarate can be taken orally to modify the immune response and reduce relapses.
- Monoclonal Antibodies: Agents like ocrelizumab and rituximab target specific immune cells to decrease inflammation and prevent disease progression.
Symptom Management
- Steroids: High-dose corticosteroids, such as prednisone, are often prescribed during relapses to reduce inflammation and speed up recovery.
- Physical and Occupational Therapy: Therapy can help maintain mobility, improve strength, and assist with daily living activities.
- Speech Therapy: This can be useful for patients experiencing difficulty with speech or swallowing.
Lifestyle and Supportive Care
Maintaining a healthy lifestyle is crucial for managing RRMS. Regular exercise, proper nutrition, stress management, and adequate sleep can all help reduce symptoms and improve overall well-being.
Prognosis and Living with Relapsing-Remitting Multiple Sclerosis
The prognosis for individuals with RRMS can vary depending on the severity of the disease, the effectiveness of treatment, and the response to therapies. With early intervention and proper treatment, many individuals with RRMS can lead relatively normal lives. However, the risk of progression to secondary progressive MS exists, and ongoing medical management is essential.
Quality of Life and Emotional Support
Living with RRMS can be challenging, particularly during relapses or if symptoms interfere with daily activities. Emotional support, counseling, and support groups can help individuals cope with the psychological and emotional aspects of the disease.
Relapsing-Remitting Multiple Sclerosis is a chronic neurological disorder that can significantly impact an individual’s quality of life. However, with the right treatment and management strategies, patients can lead fulfilling lives. Ongoing research continues to improve our understanding of the disease, paving the way for new treatments and better outcomes.