Regional anesthesia has become the standard of care for cesarean deliveries worldwide due to its superior maternal safety profile, effective analgesia, and the ability to maintain maternal consciousness during birth. Techniques such as spinal anesthesia, epidural anesthesia, and combined spinal-epidural (CSE) anesthesia are routinely employed, tailored to patient factors and clinical circumstances.

Types of Regional Anesthesia for Cesarean Delivery
Spinal Anesthesia for Cesarean Section
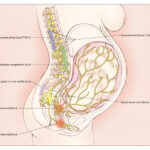
Spinal anesthesia involves a single injection of a local anesthetic, often combined with an opioid, into the subarachnoid space, resulting in rapid onset of dense sensory and motor block.
Advantages:
- Rapid onset (2–5 minutes)
- Reliable and dense block
- Minimal drug dose requirement
Disadvantages:
- Limited duration of anesthesia
- Risk of hypotension
Epidural Anesthesia for Cesarean Section
Epidural anesthesia involves catheter placement into the epidural space, allowing incremental dosing of local anesthetics and opioids.
Advantages:
- Controlled titration of block
- Extended anesthesia duration
- Postoperative analgesia through continuous infusion
Disadvantages:
- Slower onset
- Potential for incomplete block requiring supplementation
Combined Spinal-Epidural (CSE) Anesthesia
CSE anesthesia merges the benefits of spinal and epidural techniques. A spinal dose is administered for rapid onset, while the epidural catheter allows for extended anesthesia and analgesia.
Advantages:
- Rapid onset with flexibility for prolonged procedures
- Lower total dose of local anesthetics
- Option for postoperative pain management
Pharmacology of Regional Anesthesia in Cesarean Delivery
Commonly Used Agents
- Local Anesthetics: Bupivacaine, ropivacaine, lidocaine
- Opioids: Fentanyl, morphine
- Adjuvants: Epinephrine, clonidine
Drug Selection Considerations
Agent choice is based on:
- Desired duration of anesthesia
- Hemodynamic stability
- Minimization of motor block postpartum
Technical Aspects and Best Practices
Spinal Anesthesia Technique
- Positioning: Sitting or lateral decubitus
- Needle Type: Pencil-point (e.g., Whitacre or Sprotte) preferred to reduce post-dural puncture headache
- Typical Doses: 10–15 mg of hyperbaric bupivacaine with 10–25 mcg fentanyl and 100 mcg morphine
Epidural Anesthesia Technique
- Placement: Lumbar interspace L2–L4
- Test Dose: 3 mL of 1.5% lidocaine with epinephrine 1:200,000 to rule out intravascular or intrathecal placement
- Maintenance: Incremental dosing with bupivacaine or ropivacaine
Combined Spinal-Epidural Technique
- Single Interspace (Needle-Through-Needle Technique): Spinal dose administered through an epidural needle followed by epidural catheter placement
- Benefits: Immediate anesthesia with backup catheter for prolonged procedures
Benefits of Regional Anesthesia for Cesarean Section
- Maternal Safety: Lower risk of aspiration, failed intubation, and maternal morbidity compared to general anesthesia
- Fetal Benefits: Minimizes drug exposure, improving neonatal outcomes
- Immediate Maternal-Infant Bonding: Facilitates early skin-to-skin contact and breastfeeding
- Postoperative Pain Control: Epidural catheters provide excellent post-cesarean analgesia
Risks and Complications of Regional Anesthesia
Hypotension
- Most common complication
- Managed with prehydration, vasopressors (e.g., phenylephrine), and left uterine displacement
High or Total Spinal Block
- Presents with dyspnea, hypotension, and unconsciousness
- Requires immediate airway management and cardiovascular support
Post-Dural Puncture Headache (PDPH)
- Occurs in 0.1–1% of cases
- Managed conservatively or with an epidural blood patch
Infection and Hematoma
- Rare but serious
- Strict aseptic technique essential
Special Considerations in High-Risk Pregnancies
Preeclampsia and Regional Anesthesia
- Regional anesthesia preferred to avoid general anesthesia-related airway risks
- Epidural placement recommended early in labor for anticipated cesarean delivery
Cardiac Disease in Pregnancy
- Low-dose, slow-titrated epidural anesthesia minimizes hemodynamic fluctuations
Coagulopathy and Thrombocytopenia
- Platelet count >80,000/mm³ generally considered safe for neuraxial procedures
- Individualized risk assessment required
Regional Anesthesia vs General Anesthesia for Cesarean Section
| Feature | Regional Anesthesia | General Anesthesia |
|---|---|---|
| Maternal Awareness | Awake | Unconscious |
| Airway Risks | Minimal | Significant |
| Uteroplacental Perfusion | Preserved | Risk of impairment |
| Neonatal Outcomes | Superior | Risk of depression |
| Maternal Satisfaction | High | Variable |
Future Directions in Regional Anesthesia for Cesarean Section
Ultrasound-Guided Techniques
Real-time ultrasound guidance is improving the precision of neuraxial block placement, especially in obese patients or those with difficult anatomy.
Novel Adjuvants
Research continues into new additives such as dexmedetomidine and neostigmine to prolong analgesia and reduce opioid use.
Enhanced Recovery After Cesarean (ERAC) Pathways
Regional anesthesia is integral to ERAC protocols, emphasizing multimodal analgesia and rapid maternal recovery.
Regional anesthesia remains the gold standard for cesarean section anesthesia, offering superior maternal and neonatal outcomes. Mastery of spinal, epidural, and combined techniques, along with vigilant monitoring for complications, ensures safe and effective anesthesia delivery. Ongoing innovations promise further refinement and optimization of maternal care during cesarean deliveries.