Refractory osteosarcoma refers to cases where the disease persists or recurs despite initial multimodal treatment involving surgery, chemotherapy, and sometimes radiotherapy. It represents a significant clinical challenge due to limited therapeutic options and a poor overall prognosis. Most refractory cases involve either local recurrence or distant metastases, primarily to the lungs.
Pathophysiology and Mechanisms of Resistance
Osteosarcoma is characterized by a complex genetic landscape leading to intrinsic or acquired resistance mechanisms.
Genetic Alterations and Molecular Drivers
Key alterations involved include:
- p53 Mutations: Disrupt apoptosis pathways, contributing to chemoresistance.
- RB1 Inactivation: Promotes unchecked cell cycle progression.
- PI3K/AKT/mTOR Pathway Activation: Enhances tumor survival and proliferation.
- Drug Efflux Pump Upregulation: Increased expression of P-glycoprotein reduces intracellular drug concentrations.
Tumor Microenvironment Influences
The microenvironment, including hypoxia and immune evasion strategies, plays a vital role in treatment resistance, rendering standard chemotherapy less effective.
Clinical Presentation and Risk Factors for Refractory Osteosarcoma
Signs of Recurrence or Persistence
Patients with refractory osteosarcoma may present with:
- New or worsening bone pain
- Swelling or palpable masses
- Respiratory symptoms such as dyspnea or hemoptysis due to pulmonary metastases
- Pathologic fractures
Risk Factors
Several factors predispose patients to refractory disease:
- Large tumor size at diagnosis
- Axial skeleton involvement
- Poor histologic response (<90% necrosis) to neoadjuvant chemotherapy
- Presence of metastases at initial presentation
- Delay in surgical intervention
Diagnostic Evaluation of Refractory Osteosarcoma
Imaging Studies
- MRI: Preferred for local recurrence assessment.
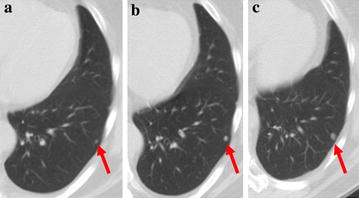
- CT Scan: Essential for detecting pulmonary metastases.
- PET-CT: Provides metabolic information and identifies distant metastases.
Biopsy and Histopathologic Confirmation
Confirmation of recurrence or refractory disease often requires a biopsy to:
- Distinguish between viable tumor and post-treatment changes
- Reassess histologic subtype
- Evaluate for secondary sarcomatous transformation
Current Treatment Strategies for Refractory Osteosarcoma
Surgical Management
Surgical resection remains a cornerstone when feasible:
- Metastasectomy: Complete surgical removal of pulmonary metastases can improve survival.
- Repeat Limb-Salvage or Amputation: Required for local recurrences when margins are compromised.
Chemotherapy Options
Second-line chemotherapy regimens offer modest benefits:
- Ifosfamide and Etoposide (IE): Commonly used salvage regimen.
- Gemcitabine and Docetaxel: Alternative with activity in resistant cases.
- High-dose Methotrexate: Considered in specific clinical scenarios.
Outcomes remain limited, with response rates typically below 20%.
Radiotherapy
Although osteosarcoma is traditionally considered radioresistant, radiotherapy can:
- Provide palliative relief
- Serve as adjuvant therapy post-resection if margins are close or positive
- Target unresectable lesions with stereotactic body radiation therapy (SBRT)
Emerging Therapeutic Approaches for Refractory Osteosarcoma
Targeted Therapies
Molecular targeting of specific pathways offers new hope:
- mTOR Inhibitors (e.g., everolimus) for tumors with PI3K/AKT/mTOR pathway activation
- Multi-kinase Inhibitors (e.g., sorafenib, regorafenib) targeting VEGFR, PDGFR, and other tyrosine kinases
- CDK4/6 Inhibitors in RB1-intact osteosarcomas
Immunotherapy Advances
Immunotherapy is emerging as a potential modality:
- Checkpoint Inhibitors: Limited success as monotherapy but promising in combination trials.
- CAR-T Cell Therapy: Investigations targeting HER2 and other osteosarcoma-associated antigens are ongoing.
Novel Chemotherapeutic Agents
Agents like liposomal doxorubicin and nanoparticle-based delivery systems are under investigation to enhance efficacy and reduce toxicity.
Prognosis and Survival Outcomes
Factors Influencing Prognosis
The following influence survival in refractory osteosarcoma:
- Achievability of complete surgical resection
- Number and location of metastatic lesions
- Interval from initial treatment to recurrence
- Response to second-line therapies
Survival Statistics
- Five-year survival for relapsed osteosarcoma is approximately 20–30%.
- Complete surgical resection of metastases significantly improves survival chances.
Future Directions in Refractory Osteosarcoma Research
Personalized Medicine and Genomic Profiling
Utilization of comprehensive genomic profiling can:
- Identify actionable mutations
- Tailor targeted therapy
- Avoid ineffective treatments
Clinical Trial Enrollment
Participation in clinical trials offers access to cutting-edge therapies and should be considered for all patients with refractory disease.
Collaborative Research Efforts
Multi-institutional consortia and international collaborations are essential to:
- Develop new therapeutic agents
- Establish standardized protocols
- Improve patient outcomes globally
Refractory osteosarcoma remains a formidable clinical challenge, requiring an individualized and aggressive multidisciplinary approach. Advancements in surgical techniques, systemic therapies, and molecular-targeted strategies are gradually improving the outlook for affected patients. Continued research and collaboration are imperative to further enhance survival and quality of life in this vulnerable population.

