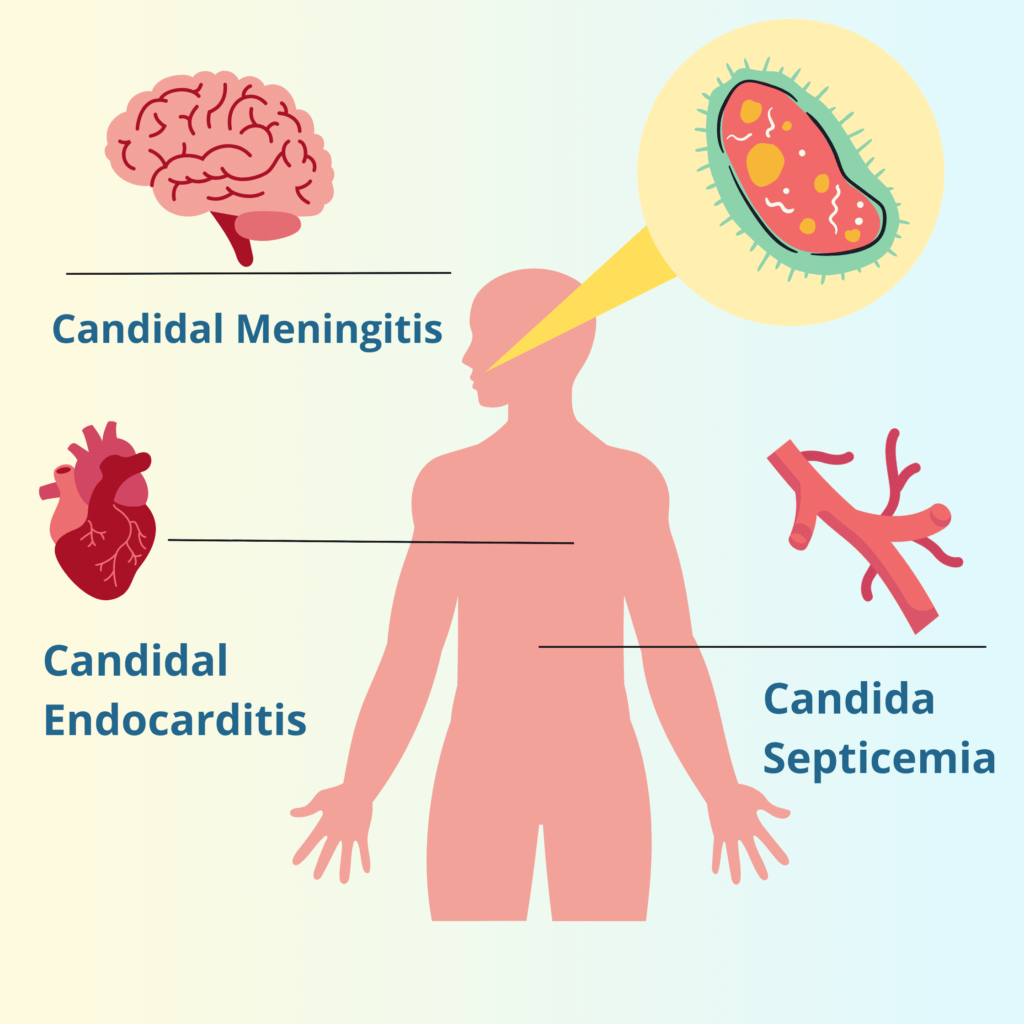
What is Candidal Septicemia?
Candidal septicemia, also known as candidemia, is a severe bloodstream infection caused by Candida species, a type of yeast that naturally resides on the skin and mucous membranes. While Candida is usually harmless in healthy individuals, it can lead to life-threatening infections when it invades the bloodstream, particularly in immunocompromised individuals or those undergoing invasive medical procedures.
Symptoms of Candidal Septicemia
Recognizing the symptoms of candidal septicemia is critical for timely diagnosis and treatment. The condition often mimics bacterial sepsis, making clinical identification challenging. Key symptoms include:
- Fever (often unresponsive to antibiotics)
- Chills and sweating
- Hypotension (low blood pressure)
- Rapid heart rate
- Fatigue and malaise
- Skin rashes or lesions (in some cases)
- Organ dysfunction (kidneys, liver, or lungs)
Causes and Risk Factors
Candidal septicemia arises when Candida enters the bloodstream, usually through breaches in natural barriers. The following are common causes and risk factors:
Common Causes:
- Invasive medical devices: Central venous catheters and other indwelling devices can act as entry points for Candida.
- Medical interventions: Prolonged hospital stays, particularly in intensive care units (ICUs), increase the risk.
- Antibiotic overuse: Broad-spectrum antibiotics can disrupt normal microbial flora, allowing Candida to overgrow.
Risk Factors:
- Immunosuppression: Patients with HIV/AIDS, cancer, or organ transplants are at higher risk.
- Chronic illnesses: Diabetes and chronic kidney disease predispose individuals to fungal infections.
- Surgery: Abdominal surgeries, especially involving perforations, can lead to candidal septicemia.
- Parenteral nutrition: Use of total parenteral nutrition (TPN) increases susceptibility.
Diagnosis
Timely diagnosis is vital for effective management. The diagnostic process includes:
- Blood Cultures: The gold standard for confirming Candida in the bloodstream. However, sensitivity may be low.
- Biomarkers: Tests like beta-D-glucan and PCR assays can aid in early detection.
- Imaging Studies: CT scans or ultrasounds may help identify the source of infection, such as abscesses or organ involvement.
- Histopathology: Tissue samples stained for fungal elements can confirm invasive Candida.
Treatment Options
Management of candidal septicemia requires prompt antifungal therapy and addressing the underlying cause. Key treatment strategies include:
Antifungal Medications:
- Echinocandins: First-line treatment due to their safety and efficacy. Examples include caspofungin and micafungin.
- Azoles: Fluconazole is often used for less severe cases or as step-down therapy.
- Amphotericin B: Reserved for refractory cases due to its toxicity.
Source Control:
- Removal of infected catheters or devices is critical to preventing persistent infection.
Supportive Care:
- Management of sepsis-related complications such as hypotension and organ dysfunction is essential.
Prevention Strategies
Preventing candidal septicemia involves reducing risk factors and improving healthcare practices. Key measures include:
- Hand Hygiene: Strict adherence to hand hygiene protocols in healthcare settings.
- Device Management: Minimize the use and duration of central venous catheters and other invasive devices.
- Antimicrobial Stewardship: Rational use of antibiotics to prevent Candida overgrowth.
- Prophylactic Antifungals: For high-risk patients, targeted prophylaxis can reduce incidence.
Prognosis and Complications
The prognosis of candidal septicemia depends on early diagnosis and effective management. Untreated cases have a high mortality rate, often exceeding 40%. Potential complications include:
- Septic Shock: Life-threatening drop in blood pressure.
- Multiorgan Failure: Common in severe infections.
- Endophthalmitis: Fungal infection of the eye leading to vision loss.