Refractory aspergillosis refers to invasive aspergillosis (IA) that fails to respond to standard first-line antifungal therapy, typically voriconazole or other triazoles. This serious, life-threatening condition predominantly affects immunocompromised individuals, including patients with hematologic malignancies, organ transplants, or prolonged neutropenia. Early recognition and aggressive management are critical to improving survival rates.
Pathogenesis and Risk Factors
The pathogenic mold Aspergillus invades host tissues when immune defenses are impaired. In refractory cases, persistent infection occurs despite antifungal treatment, often due to:
- Antifungal Resistance: Mutation-driven azole resistance in Aspergillus fumigatus strains.
- Delayed Diagnosis: Advanced infection before initiation of therapy.
- Host Factors: Profound immunosuppression, graft-versus-host disease, or ongoing corticosteroid therapy.
- Pharmacokinetics Issues: Subtherapeutic antifungal drug levels due to poor absorption or drug interactions.
Understanding these risk factors is paramount to tailoring effective intervention strategies.
Clinical Presentation of Refractory Aspergillosis
Symptoms of refractory aspergillosis are non-specific and often overlap with other invasive fungal infections. Key clinical features include:
- Persistent fever unresponsive to broad-spectrum antibiotics and antifungal therapy.
- Worsening respiratory symptoms, such as cough, hemoptysis, or pleuritic chest pain.
- Progressive pulmonary infiltrates or nodules on imaging despite treatment.
- Signs of dissemination to the central nervous system, skin, or other organs in advanced cases.
Timely recognition of clinical deterioration is essential to prompt a reevaluation of therapeutic strategies.
Diagnostic Approach to Refractory Aspergillosis
Confirming refractory disease requires a comprehensive and methodical approach.
Imaging Studies
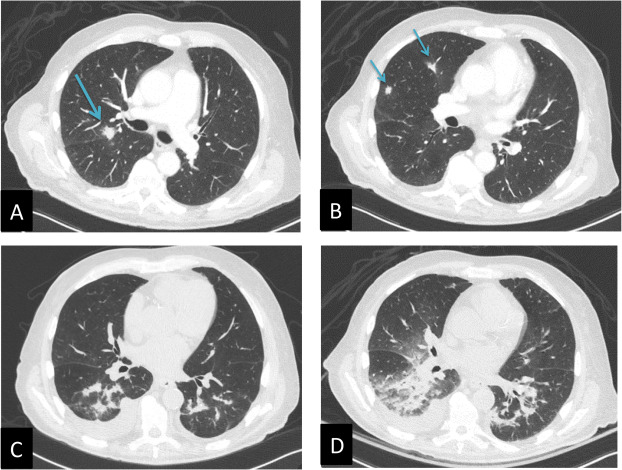
- High-Resolution CT (HRCT) Scans: Show persistent or progressive lung lesions, halo signs, or cavitary changes.
- MRI: Useful for identifying CNS involvement.
Microbiological and Molecular Testing
- Culture and Histopathology: Definitive diagnosis through tissue samples remains crucial.
- Galactomannan Assay: Monitoring serum or BAL galactomannan levels helps assess fungal burden.
- PCR Testing: Detects Aspergillus DNA with high sensitivity and supports diagnosis.
Antifungal Susceptibility Testing
Evaluating antifungal resistance profiles guides modification of therapeutic regimens, especially in regions with known high azole resistance rates.
Therapeutic Strategies for Refractory Aspergillosis
Management of refractory aspergillosis demands an aggressive, multifaceted approach.
Salvage Antifungal Therapy
Salvage therapy involves switching to or combining antifungal agents different from the initial therapy:
- Lipid Formulations of Amphotericin B: Broad-spectrum fungicidal activity; preferred in critically ill patients.
- Isavuconazole: A second-generation triazole with broad coverage and favorable safety profile.
- Posaconazole: Effective against resistant Aspergillus strains; available in delayed-release tablets for improved absorption.
- Combination Therapy: Evidence suggests that combining a triazole with an echinocandin (e.g., caspofungin) may offer synergistic effects in refractory cases.
Drug choice should be guided by susceptibility data, clinical severity, and patient-specific factors such as renal or hepatic function.
Immunomodulatory Strategies
Enhancing host immunity is critical, particularly in severely immunocompromised patients:
- Reduction of Immunosuppression: Tapering corticosteroids or modifying immunosuppressive regimens when feasible.
- Granulocyte Transfusions: Considered in patients with profound neutropenia.
- Use of Immunomodulatory Agents: Agents such as interferon-gamma have shown potential benefits in limited cases.
Surgical Intervention
Surgical resection may be warranted for localized pulmonary lesions, massive hemoptysis, or in cases with fungal balls (aspergilloma) that are refractory to medical therapy.
Emerging Therapies and Future Directions
Research continues to seek novel approaches for the management of refractory aspergillosis:
- New Antifungal Agents: Olorofim, a first-in-class orotomide, is showing promise in clinical trials for azole-resistant aspergillosis.
- Immunotherapies: Monoclonal antibodies targeting fungal components and vaccines are under investigation.
- Adjunctive Therapies: Use of iron chelators and inhibitors of fungal stress response pathways are being explored to enhance antifungal efficacy.
Continued innovation is critical to improving outcomes in this challenging patient population.
Prognosis of Refractory Aspergillosis
The prognosis for refractory aspergillosis remains guarded, with reported mortality rates exceeding 50% in some cohorts. Early recognition, rapid diagnostic evaluation, appropriate antifungal salvage therapy, and aggressive supportive care are essential to optimizing survival outcomes.
Patients surviving refractory aspergillosis often require prolonged antifungal therapy and close clinical and radiological monitoring to detect recurrences or complications.
Refractory aspergillosis represents one of the most formidable challenges in infectious disease management, particularly in immunocompromised hosts. Through timely diagnosis, strategic use of salvage antifungal therapies, immunomodulation, and when necessary, surgical intervention, we can significantly improve patient outcomes. Continued research into novel therapeutics and a multidisciplinary treatment approach remain the cornerstones for managing this severe fungal infection effectively.