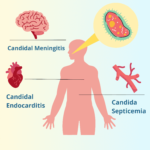
Candidal meningitis is a rare but severe form of fungal meningitis caused by Candida species, most commonly Candida albicans. This condition primarily affects immunocompromised individuals and presents significant diagnostic and therapeutic challenges. Timely identification and treatment are critical to improving outcomes.

Causes and Risk Factors
Etiology
Candidal meningitis results from the dissemination of Candida species, which are opportunistic fungi that commonly inhabit the skin, gastrointestinal tract, and mucous membranes.
Key Risk Factors
- Immunocompromised States: Conditions such as HIV/AIDS, cancer, and organ transplantation increase susceptibility.
- Neonatal Risk: Premature infants are at higher risk due to underdeveloped immune systems.
- Medical Interventions: Indwelling medical devices like central venous catheters and neurosurgical procedures can facilitate fungal entry.
- Prolonged Antibiotic Use: Disruption of normal flora by antibiotics may promote fungal overgrowth and dissemination.
Pathophysiology
Upon entering the bloodstream, Candida can breach the blood-brain barrier, leading to inflammation of the meninges. The infection results in a cascade of immune responses, which, if untreated, can cause significant neurological damage.
Clinical Manifestations
Common Symptoms
- Persistent headache
- Fever
- Nausea and vomiting
- Neck stiffness
- Altered mental status
Advanced Symptoms
- Seizures
- Focal neurological deficits
- Coma in severe cases
Symptoms often mimic bacterial meningitis, complicating initial diagnosis.
Diagnosis
Laboratory Investigations
- Cerebrospinal Fluid (CSF) Analysis:
- Elevated protein levels
- Decreased glucose concentrations
- Presence of yeast cells or pseudohyphae on microscopy
- Culture: Isolation of Candida species from CSF confirms the diagnosis.
Imaging Studies
- MRI or CT Scans: Detect structural abnormalities such as abscesses or hydrocephalus.
Serological Tests
- β-D-Glucan Assay: A marker for invasive fungal infections.
- Candida Antigen Testing: Useful for rapid diagnosis.
Treatment
Antifungal Therapy
- First-Line Treatment: Liposomal Amphotericin B combined with flucytosine.
- Step-Down Therapy: Oral fluconazole for long-term maintenance.
Supportive Care
- Management of intracranial pressure
- Treatment of seizures
- Nutritional and hydration support
Surgical Interventions
In cases of hydrocephalus or abscess formation, neurosurgical procedures may be required.
Prognosis
The prognosis of candidal meningitis depends on early diagnosis and treatment. Delayed intervention often results in poor outcomes, including permanent neurological damage or death. Mortality rates range from 30% to 50% in severe cases.
Prevention
Preventive Measures
- Strict aseptic techniques during medical interventions.
- Prophylactic antifungals for high-risk patients.
- Monitoring for early signs of infection in immunocompromised individuals.