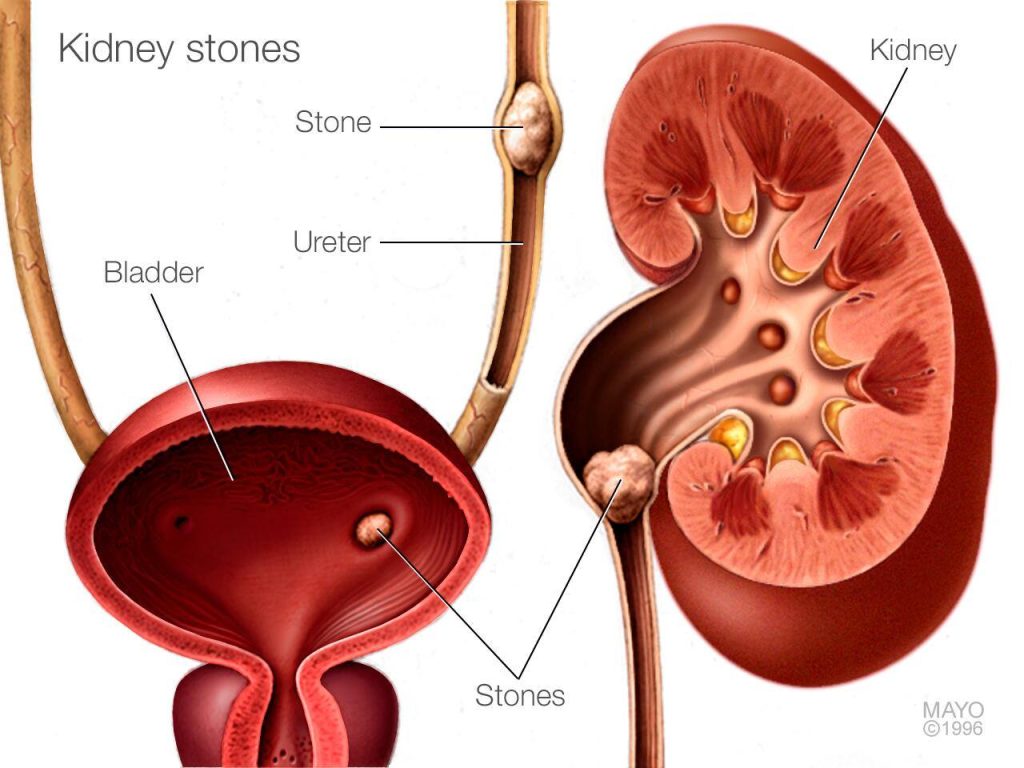
Recurrent calcium renal calculi, commonly referred to as recurring kidney stones, are solid deposits predominantly composed of calcium oxalate or calcium phosphate. These stones form within the kidneys and can lead to significant morbidity due to pain, urinary tract obstruction, and potential renal impairment. Managing recurrent cases demands a comprehensive understanding of underlying etiologies, effective diagnostic evaluation, and long-term preventive strategies.
Causes and Risk Factors for Recurrent Calcium Renal Calculi
Multiple metabolic, dietary, and anatomical factors contribute to the development of recurrent calcium renal calculi:
- Hypercalciuria: Excessive urinary calcium excretion, often idiopathic or secondary to systemic conditions like hyperparathyroidism.
- Hyperoxaluria: Elevated urinary oxalate levels from dietary sources or gastrointestinal disorders.
- Hypocitraturia: Reduced citrate in urine, decreasing stone-inhibitory effects.
- Dehydration: Insufficient fluid intake leads to concentrated urine, promoting crystal aggregation.
- Dietary Factors: High intake of oxalate-rich foods (e.g., spinach, nuts), sodium, and animal proteins.
- Genetic Predisposition: Familial clustering suggests hereditary influences.
- Anatomical Abnormalities: Obstructions or stasis within the urinary tract predispose individuals to stone formation.
Pathophysiology of Calcium Stone Formation
The formation of calcium stones is a multistep process involving supersaturation of urine with stone-forming constituents, nucleation, crystal growth, aggregation, and retention in the renal tubules or pelvis.
Clinical Manifestations of Recurrent Calcium Renal Calculi
Patients with recurrent calcium renal calculi often present with:
- Renal Colic: Sudden, severe flank pain radiating to the groin.
- Hematuria: Presence of blood in urine, either gross or microscopic.
- Dysuria and Urgency: When stones obstruct lower urinary tract pathways.
- Nausea and Vomiting: Common due to severe pain.
- Urinary Tract Infections: Secondary infections may complicate stone disease.
The recurrent nature increases the risk of progressive renal damage if left untreated.
Diagnostic Evaluation for Recurrent Calcium Renal Calculi
Accurate diagnosis and metabolic evaluation are essential for targeted prevention:
Imaging Studies
- Non-Contrast Helical CT Scan: Gold standard for detecting stones.
- Ultrasound: Useful for initial assessment, especially in pregnant women or those avoiding radiation.
- Plain Radiography (KUB): Effective for radiopaque stones but less sensitive overall.
Laboratory Investigations
- Urinalysis: Detection of hematuria, crystals, and signs of infection.
- 24-Hour Urine Collection: Assessment of urinary calcium, oxalate, citrate, uric acid, sodium, and volume.
- Blood Tests: Evaluation of serum calcium, phosphate, uric acid, parathyroid hormone levels, and renal function.
Comprehensive metabolic workup is essential to identify modifiable risk factors.
Management Strategies for Recurrent Calcium Renal Calculi
Management aims at treating existing stones, preventing recurrence, and correcting underlying metabolic abnormalities.
Acute Stone Management
- Pain Control: NSAIDs are first-line; opioids may be needed for severe cases.
- Hydration Therapy: Encouragement of high fluid intake to facilitate stone passage.
- Medical Expulsive Therapy: Alpha-blockers (e.g., tamsulosin) promote stone expulsion.
Stone Removal Procedures
- Extracorporeal Shock Wave Lithotripsy (ESWL): Non-invasive fragmentation of stones.
- Ureteroscopy: Endoscopic retrieval or fragmentation.
- Percutaneous Nephrolithotomy: Reserved for large or complex stones.
Long-Term Prevention of Recurrent Calcium Stones
Preventive strategies play a pivotal role in managing recurrent calcium renal calculi:
Dietary Modifications
- Increased Fluid Intake: Aim for urine output exceeding 2.5 liters daily.
- Reduced Sodium Consumption: Sodium promotes calciuria; dietary restriction is crucial.
- Adequate Dietary Calcium: Contrary to intuition, dietary calcium binds oxalate in the gut and prevents absorption.
- Limit Oxalate-Rich Foods: Spinach, beets, nuts, chocolate, and tea.
- Moderate Animal Protein Intake: Excessive intake increases urinary calcium and decreases citrate.
Pharmacologic Therapy
- Thiazide Diuretics: Reduce urinary calcium excretion.
- Potassium Citrate: Corrects hypocitraturia and alkalinizes urine.
- Allopurinol: Useful in patients with concurrent hyperuricosuria.
- Vitamin B6: Reduces endogenous oxalate production in specific cases.
Ongoing monitoring with periodic 24-hour urine studies and imaging is recommended to assess therapy efficacy and adjust interventions.
Complications of Untreated Recurrent Calcium Renal Calculi
Failure to manage recurrent stones can result in:
- Chronic Kidney Disease: Progressive nephron loss from recurrent obstruction and infections.
- Recurrent Urinary Tract Infections: Potential for pyelonephritis or urosepsis.
- Nephrocalcinosis: Diffuse renal parenchymal calcification leading to renal dysfunction.
- Persistent Pain and Disability: Impacting quality of life and work productivity.
Timely intervention significantly reduces morbidity associated with recurrent stones.
Recurrent calcium renal calculi represent a significant clinical challenge requiring a multidisciplinary approach encompassing acute management, detailed metabolic evaluation, patient education, and long-term preventive strategies. Through diligent implementation of tailored interventions, we can markedly reduce recurrence rates, preserve renal function, and improve patient outcomes.