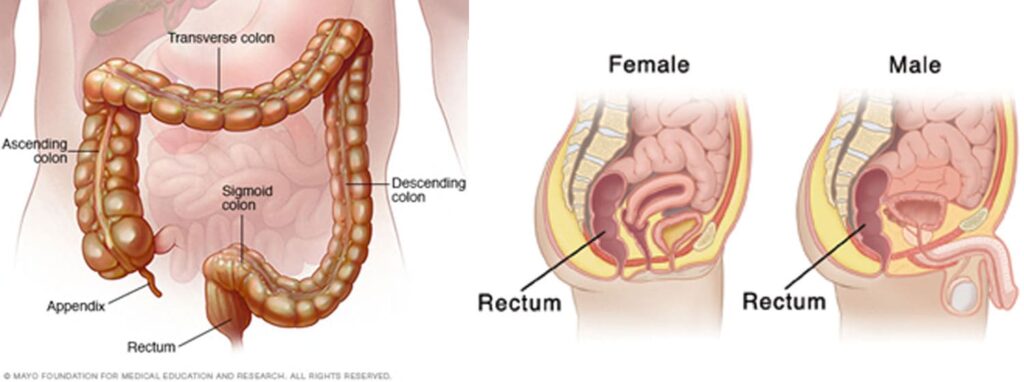
Rectal pain refers to discomfort or pain originating from the rectal or anal regions. It can be acute or chronic, sharp or dull, and may vary in intensity. Due to its diverse causes, rectal pain requires thorough evaluation to ensure effective management and prevent serious complications.
Common Causes of Rectal Pain
Several conditions can result in rectal pain, ranging from benign issues to serious medical concerns:
- Anal Fissures: Small tears in the anal lining, often causing sharp pain during or after bowel movements.
- Hemorrhoids: Swollen veins in the rectum or anus leading to aching or throbbing pain, particularly during sitting or defecation.
- Proctitis: Inflammation of the rectal lining due to infections, inflammatory bowel diseases, or radiation therapy.
- Abscesses and Fistulas: Infected cavities and abnormal connections causing severe pain, swelling, and possible fever.
- Anorectal Cancer: Malignant tumors in the rectum or anus presenting as persistent pain, often accompanied by bleeding.
- Levator Ani Syndrome: Chronic muscle spasm in the pelvic floor muscles resulting in intermittent rectal pain.
- Proctalgia Fugax: Sudden, severe episodes of rectal pain lasting from seconds to minutes, with no identifiable cause.
Other causes include sexually transmitted infections, trauma, or postoperative complications.
Symptoms Associated with Rectal Pain
Rectal pain can present with various associated symptoms depending on the underlying cause:
- Bleeding from the anus
- Mucous discharge
- Constipation or diarrhea
- Sensation of incomplete bowel emptying
- Swelling or lump formation
- Fever and chills in cases of infection
- Radiating pain to the lower back or pelvis
Recognizing accompanying symptoms aids in narrowing the differential diagnosis.
Pathophysiology of Rectal Pain Conditions
Different pathological mechanisms contribute to rectal pain:
Inflammatory, infectious, neoplastic, and mechanical processes each impact the rectal and anal structures, resulting in distinct pain patterns.
Diagnostic Evaluation of Rectal Pain
A systematic approach is essential for accurate diagnosis:
- Detailed Medical History: Nature, duration, and pattern of the pain, associated symptoms, and relevant risk factors.
- Physical Examination: Inspection and digital rectal examination to detect fissures, masses, abscesses, or hemorrhoids.
- Anoscopy and Proctoscopy: Direct visualization of the rectal and anal canal.
- Imaging Studies:
- MRI or endorectal ultrasound for deep-seated abscesses or tumors.
- CT scan if abscess or fistula formation is suspected.
- Laboratory Testing: Infections and inflammatory markers.
- Colonoscopy: Indicated if cancer, polyps, or inflammatory bowel disease is suspected.
A comprehensive diagnostic strategy ensures that serious causes are not overlooked.
Management and Treatment Strategies for Rectal Pain
Treatment depends on the underlying etiology:
- Anal Fissures:
- High-fiber diet, stool softeners, topical anesthetics, and sitz baths.
- In refractory cases, nitroglycerin ointments or surgical interventions like lateral internal sphincterotomy.
- Hemorrhoids:
- Conservative therapy with fiber supplementation and topical treatments.
- Rubber band ligation, sclerotherapy, or surgical hemorrhoidectomy for severe cases.
- Proctitis:
- Antibiotics for infectious causes.
- Anti-inflammatory medications for inflammatory bowel disease-related proctitis.
- Abscesses and Fistulas:
- Surgical drainage and fistula repair.
- Pelvic Floor Dysfunction:
- Physical therapy, biofeedback, and muscle relaxants.
- Cancer:
- Multimodal approach involving surgery, chemotherapy, and radiation therapy based on staging.
Pain control measures, including NSAIDs, topical analgesics, and, if necessary, opioids, are incorporated judiciously.
Complications Arising from Untreated Rectal Pain
Ignoring rectal pain can lead to severe complications:
- Chronic pain syndromes
- Infections spreading to deeper tissues
- Anorectal abscess rupture
- Fistula formation
- Malignancy progression
Timely intervention prevents the escalation of potentially life-threatening conditions.
Prevention of Rectal Pain
Effective preventive strategies include:
- Maintaining a high-fiber diet to prevent constipation and straining
- Adequate hydration
- Practicing safe anal intercourse
- Avoiding prolonged sitting
- Regular medical screenings for at-risk individuals
- Prompt treatment of anorectal disorders
Lifestyle adjustments play a critical role in minimizing the risk of developing rectal pain.
Rectal pain is a multifaceted condition necessitating careful evaluation and targeted treatment. We must prioritize accurate diagnosis, tailored management, and preventive strategies to ensure optimal outcomes for patients experiencing this distressing symptom. Early recognition and intervention not only relieve discomfort but also avert serious complications associated with underlying anorectal diseases.