Rectal gonorrhea is a sexually transmitted infection caused by Neisseria gonorrhoeae, a Gram-negative diplococcus. It primarily affects the rectal mucosa following receptive anal intercourse or, less commonly, autoinoculation from genital infections. Many cases are asymptomatic, allowing for silent transmission and delayed diagnosis, increasing the risk of complications.
Causes and Risk Factors of Rectal Gonorrhea
Transmission occurs through direct mucosal contact with infected secretions during unprotected anal sex. Additional risk factors include:
- Multiple sexual partners
- Men who have sex with men (MSM)
- Inconsistent condom use
- Concurrent sexually transmitted infections
- Immunosuppression
The organism targets columnar epithelial cells, initiating an inflammatory response that leads to mucosal damage and symptom development.
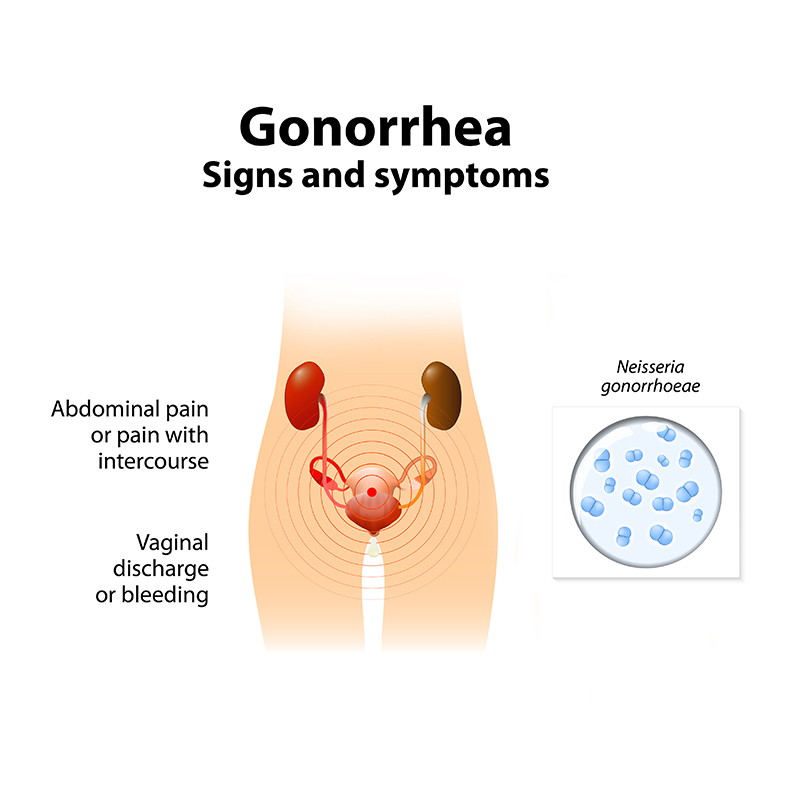
Clinical Manifestations: Signs and Symptoms of Rectal Gonorrhea
Rectal gonorrhea often presents subtly but can include:
- Rectal pain or discomfort
- Mucoid, purulent, or bloody rectal discharge
- Tenesmus (urge to defecate with little stool passage)
- Itching or irritation of the anus
- Diarrhea or altered bowel habits
- Rectal bleeding
Severe cases may be mistaken for inflammatory bowel disease, complicating the diagnostic process.
Pathogenesis of Rectal Gonorrhea Infection
Following exposure, N. gonorrhoeae adheres to and invades the rectal epithelium, triggering a local immune response. The resulting inflammation can range from mild mucosal irritation to severe ulceration and tissue necrosis.
Diagnostic Approach to Rectal Gonorrhea
Timely diagnosis is essential to prevent complications and further spread:
- Nucleic Acid Amplification Tests (NAATs): Highly sensitive and specific, performed on rectal swabs.
- Culture Methods: Useful for antimicrobial susceptibility testing.
- Physical Examination: Anoscopy may reveal mucosal erythema, discharge, or ulcerations.
- Comprehensive STI Screening: Concurrent testing for chlamydia, syphilis, and HIV is recommended.
Accurate and early diagnosis ensures effective treatment and minimizes transmission risks.
Management and Treatment of Rectal Gonorrhea
Effective treatment requires antibiotics active against N. gonorrhoeae:
- First-line Treatment:
- Ceftriaxone 500 mg intramuscularly in a single dose.
- Doxycycline 100 mg orally twice daily for 7 days if concurrent chlamydia infection is not excluded.
- Antimicrobial Resistance Considerations:
- Resistance testing is crucial in persistent or recurrent infections.
- Alternative regimens may be considered based on susceptibility patterns.
Sexual partners from the preceding 60 days must be notified, tested, and treated as necessary. Sexual activity should be avoided for at least 7 days after completion of treatment and resolution of symptoms.
Potential Complications of Untreated Rectal Gonorrhea
Failure to diagnose and treat rectal gonorrhea can lead to serious consequences:
- Chronic proctitis
- Perirectal abscess formation
- Fistula development
- Systemic dissemination causing arthritis, tenosynovitis, or dermatitis (Disseminated Gonococcal Infection, DGI)
- Increased HIV transmission risk
Proactive management is critical to prevent these severe outcomes.
Prevention Strategies for Rectal Gonorrhea
Comprehensive prevention efforts include:
- Consistent and correct condom use during anal intercourse
- Regular STI screenings, particularly for high-risk populations
- Reduction of sexual partners
- Prompt treatment of infections to prevent transmission
- Education on safe sexual practices
Public health initiatives targeting awareness and prevention significantly reduce rectal gonorrhea incidence.
Rectal gonorrhea, though often asymptomatic, poses significant health risks if left untreated. Through vigilant screening, prompt diagnosis, and appropriate antibiotic therapy, we can effectively manage and prevent this common yet serious sexually transmitted infection. Strong public health strategies and personal protective measures remain crucial in controlling its spread.