Rectal chlamydia trachomatis infection is a sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis, affecting the rectal mucosa. It often results from receptive anal intercourse but can also occur through autoinoculation. Rectal chlamydia can be asymptomatic or present with significant proctitis symptoms, necessitating prompt diagnosis and treatment to avoid severe complications.
Causes and Transmission of Rectal Chlamydia
Chlamydia trachomatis is primarily transmitted through unprotected anal sex with an infected partner. It may also spread via contaminated fingers or sex toys. Factors increasing the risk include:
- Engaging in receptive anal intercourse
- Multiple sexual partners
- Inconsistent condom use
- Previous history of sexually transmitted infections
The bacterium invades epithelial cells, causing localized inflammation and cellular damage, leading to clinical symptoms.
Clinical Presentation: Recognizing Symptoms of Rectal Chlamydia
While many individuals remain asymptomatic, symptomatic infections commonly present as:
- Rectal pain and discomfort
- Mucoid or bloody rectal discharge
- Tenesmus (feeling of incomplete evacuation)
- Diarrhea or constipation
- Rectal bleeding
- Anal itching or irritation
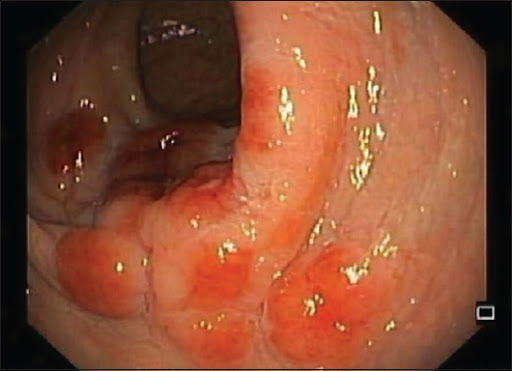
Severe cases may mimic inflammatory bowel disease, making clinical suspicion critical for proper diagnosis.
Pathophysiology of Rectal Chlamydia Infection
Once Chlamydia trachomatis infects the rectal mucosa, it triggers an inflammatory response characterized by infiltration of immune cells and mucosal ulceration. Chronic infection without treatment may lead to fibrosis, stricture formation, or an increased risk of secondary infections.
Diagnostic Evaluation of Rectal Chlamydia
Accurate diagnosis is essential for effective management and includes:
- Nucleic Acid Amplification Tests (NAATs): The gold standard for detecting C. trachomatis DNA from rectal swabs.
- Rectal Swab Collection: Proper technique ensures the highest sensitivity.
- Symptom Assessment: Evaluation of rectal discomfort, discharge, or bleeding.
- Additional STI Screening: Concurrent testing for other STIs such as gonorrhea, syphilis, and HIV is recommended.
Prompt identification enables early treatment and limits transmission to partners.
Management and Treatment of Rectal Chlamydia
Treatment regimens must eradicate the infection completely:
- First-line Therapy:
- Doxycycline 100 mg orally twice daily for 7 days.
- Alternative Therapy:
- Azithromycin 1 g orally in a single dose (less preferred for rectal infections due to reduced efficacy).
Partner notification and treatment are crucial to prevent reinfection. Patients should abstain from sexual activity until 7 days after completing therapy and resolution of symptoms.
Potential Complications of Untreated Rectal Chlamydia
Failure to treat rectal chlamydia can result in:
- Chronic proctitis
- Rectal strictures
- Fistula formation
- Increased susceptibility to HIV
- Dissemination leading to lymphogranuloma venereum (LGV) in certain strains
Early detection and adherence to treatment significantly reduce the risk of these adverse outcomes.
Prevention Strategies for Rectal Chlamydia Infection
Effective prevention measures include:
- Consistent use of condoms or dental dams during anal intercourse
- Regular STI screenings for sexually active individuals
- Reduction of sexual partners
- Prompt treatment of infected individuals and their partners
- Avoidance of sharing sex toys without proper cleaning
Public health campaigns emphasizing safe sex practices play a vital role in reducing the incidence of rectal chlamydia.
Rectal chlamydia trachomatis infection remains a significant public health concern, particularly among populations engaging in receptive anal intercourse. Vigilance in screening, early diagnosis, and effective treatment are critical to prevent complications and transmission. Adherence to prevention strategies and public awareness can markedly decrease the burden of this often asymptomatic but potentially serious infection.